Physiotherapy versus Advice for Chronic Whiplash

Introduction
Today we review an article from a while ago by Michaleff et al. from 2014. This study was set up to learn whether a comprehensive physiotherapy-led intervention was better than a brief period of advice in chronic whiplash patients. Earlier trials had found no beneficial effect in acute whiplash, but there was not a lot of robust evidence available in chronic whiplash. As chronic whiplash-associated disorders account for a large proportion of healthcare costs, this study is relevant to determine the impact of physiotherapy. As such, the current study examines physiotherapy versus advice for chronic whiplash.
Methods
A pragmatic two-group randomized controlled trial was set up. Eligible participants were between 18-65 years and had sustained a grade 1 or 2 whiplash for at least 3 months. They had at least a moderate limitation in their activities due to their pain (determined by the Short Form 36 survey) or moderate pain levels.
The intervention group received an individually tailored exercise program which was held twice a week for 8 weeks and once per week for 4 weeks. In total, there were 20 sessions, which were all supervised by the physiotherapist and lasted for 1 hour. In the first four weeks,
specific cervical spine exercises were performed. These included craniocervical flexion exercises, neck extensor exercises, scapular training, postural re-education, and sensorimotor exercises. In the first week, the exercises could be supplemented with manual therapy techniques (excluding manipulations). During weeks 4 to 6, the exercises progressed to an integration of the specific neck exercises into functional exercises. Thereafter, graded activity was used to help participants achieve their set goals. Here, upper and lower limb strengthening and endurance exercises were used and specific functional tasks were practiced. Additionally, from the first to the last week, aerobic exercise was prescribed. Further, the participants from this group received a 12-week home exercise program.
The control group received a patient educational booklet which served as a management guide. You can find the booklet by following this link. This booklet was given to the participants during a 30-minute consultation with a physiotherapist. In this session, the participants read the booklet and were allowed to ask questions. The exercises were practiced with minimal guidance from the physiotherapist. Then they were instructed to implement the advice and do the exercises at home. They had the opportunity to have 2 telephone calls with the physiotherapist to clarify their questions.
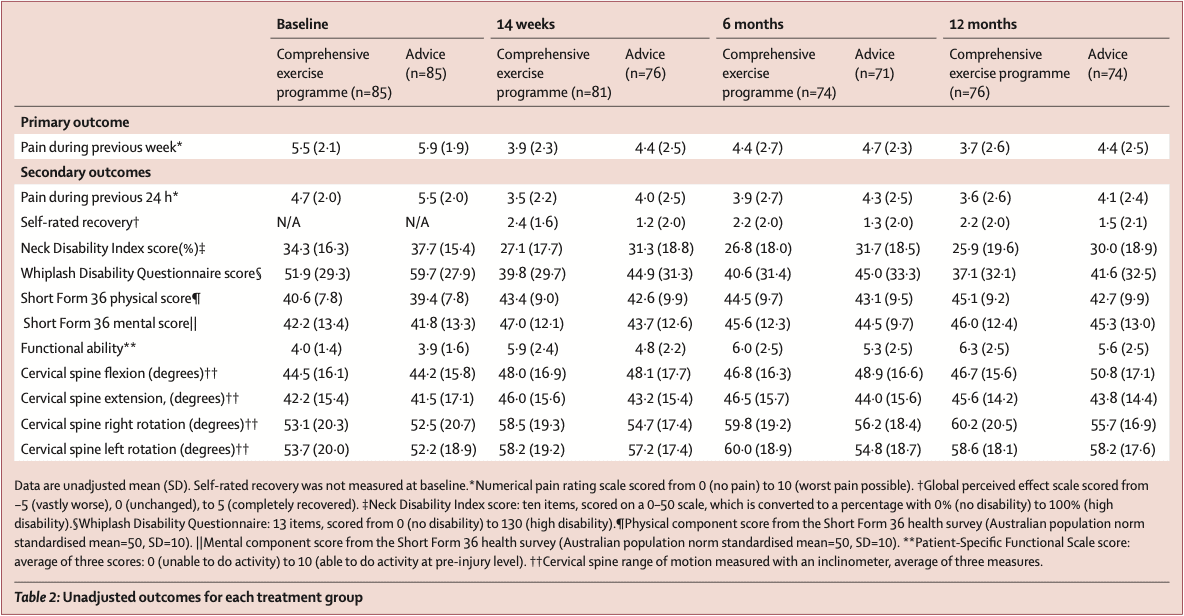
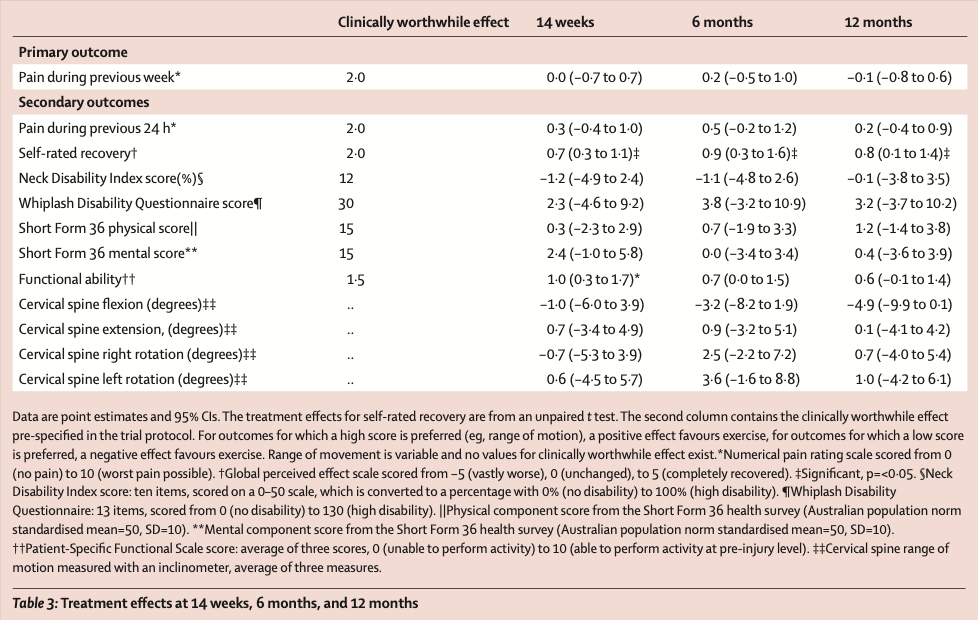
The primary outcome of interest was the average pain intensity during the preceding week on a 0-10 numeric rating scale which was captured at baseline, 14 weeks, 6 months, and 12 months.
Results
The trial included 86 participants in each group. The follow-up revealed good retention of participants in the trial. At 14 weeks, 6 months, and 12 months, respectively 91%, 84%, and 87% of participants were analyzed. The characteristics of the included participants show that most participants were middle-aged females who had symptoms for nearly 2 years. Most of the sample was eligible for compensation and about a third had settled a claim.
Compliance was good, with the median number of treatment sessions attended being 17 out of 20 sessions maximum. The analysis revealed that the intervention group had no better outcomes in the primary, or secondary analyses. This means that the comprehensive physiotherapy protocol was no better than the advice.
Questions and thoughts
I often question myself why some interventions are better than others. Generally speaking, a lot of trials show effective interventions as they include exercise training, combined or not with good advice, coaching, and progressively reintroducing the individual to desired tasks/sports. Most of the time, the interventions are good because they are specific to one’s injury, progressive in time, or held frequently, allowing the individual to recover. In trials such as this, where such an intervention was compared to a very brief control intervention, most of the time we would expect the intervention to outperform the control group because they are simply doing more. In this trial, this was not the case.
What may have caused the lack of finding a relevant benefit from such a comprehensive intervention? Maybe the outcome measure was not the best suited. At least moderate pain levels were required to participate in the present study but a clinically important difference was determined to be at least 2 points on the NRS scale. The baseline pain levels were 5.5 and 5.9 out of 10 for the intervention and control groups respectively. We know that it is more likely to find important reductions in pain when the initial pain scores are high (regression to the mean).
Another potential contributing factor to the lack of important outcomes may lie in the fact that the average pain intensity during the preceding week is an outcome that may be subject to recall bias, and patients may over- or underestimate their levels of pain when asked about the previous week. Do you remember what you ate last Tuesday? Furthermore, in chronic pain, the recommendation is to avoid focusing on pain specifically but to give more attention to someone’s functional capacities. If you can improve their level of functioning, they will get a lot better in general, despite having some levels of persisting pain.
Something to ask yourself is whether the patient in front of you may benefit from not recovering. Especially when they have settled a claim. Indeed, not everyone will receive compensation, but when someone has the chance, they will most likely try. This is a potential black flag. The fact that a third of participants had settled a claim and more people were eligible for receiving compensation than were not, may be another potential explanation. The authors state: “The subjective nature of whiplash-associated disorders means that in some societies the injury is associated with suspicion of malingering and fraudulent insurance claims.” However, neither the subjective nor the objective outcomes were improving, so the authors find malingering unlikely. Something to think of…
Talk nerdy to me
The sample size was calculated appropriately and required 172 participants to be included in the trial. The results reveal no clinically important differences in the primary and secondary outcomes. Thereby this study is in accordance with the conclusions of the UK MINT trial. The authors point to the possibility of nociceptive hyperexcitability and post-traumatic stress symptoms influencing (the lack) of relevant outcomes in this condition.
Take home messages
This 2014 trial showed no beneficial effects of physiotherapy versus advice for chronic whiplash. This was further supported by evidence in 2017 from Griffin et al. They found no clinically meaningful differences between comprehensive exercise programs, which included general exercise, and minimal intervention controls in the medium and long term. Further research on how to effectively manage patients with chronic whiplash-associated symptoms is thus advocated.
Reference
Additional reference
100% FREE HEADACHE HOME EXERCISE PROGRAM
Download this FREE home exercise program for your patients suffering from headaches. Just print it out and hand it to them for them to perform these exercises at home