Nerve-Related Cervicobrachial Pain: Effectiveness of Neural Mobilizations

Introduction
A common complication of neck pain is the co-occurrence of arm pain. Nerve-related cervicobrachial pain is a type of arm pain that arises from increased mechanosensitivity along the nerve or nerve root. Nerve-related cervicobrachial pain can involve various presentations, from true radiculopathy with objective neurological deficits to heightened neural mechanosensitivity without nerve damage. Neural mobilizations are designed to mobilize the nervous system itself and facilitate movement between neural structures and surrounding tissues. Previous research has not looked into subgroups of patients with different drivers of their cervicobrachial pain, and this study wanted to fill that gap.
Methods
This systematic review, published in 2024, included randomized controlled trials (RCTs) that studied the effect of neural mobilizations on pain or disability in individuals with nerve-related cervicobrachial pain. The included studies were classified based on the underlying presentations of the nerve-related cervicobrachial pain into:
-
- Painful cervical radiculopathy: in case signs of nerve-conduction loss are present. For example, myotomal weakness or dermatomal sensory loss
- Wainner cluster: 3 out of 4 positive tests from the following:
- Upper limb neurodynamic test
- Ipsilateral cervical rotation range of motion < 60°
- Distraction test relieves the complaints
- Spurling test reproducing the typical symptoms
- Hall and Elvey Cluster
-
-
- Reduced active or passive cervical range of motion
- Evidence of heightened neural mechanosensitivity by a positive upper limb neurodynamic test
- Local cervical dysfunction objectified by intervertebral movement testing
-
- Other
The effect of neural mobilizations was expressed as a mean difference and interpreted according to the minimal clinically important difference (MCID). A mean difference was classified as small if it was below the MCID, moderate if just above the MCID, or large if greater than twice the MCID. For pain intensity, the MCID was defined as 1.3 out of 10 points on a VAS scale, while disability required 10 points on the 0-100 Neck Disability Index. In case different outcome measures were combined, a summary standardized mean difference was calculated and interpreted as small (0.20-0.50), moderate (0.50-0.80), or large (>0.80).
Results
Of 16.376 screened records, 27 studies met the inclusion criteria and were included in the systematic review. All included studies were RCTs assessing the effectiveness of neural mobilizations, and most of them compared the effect of these neural mobilizations as an adjuvant to standard physiotherapy compared to standard physiotherapy alone. Other comparators included cervical traction, neck exercises, McKenzie manipulation/exercise, Mulligan and Maitland cervical mobilizations, ultrasound, laser, and oral ibuprofen. Three studies compared neural mobilizations to no treatment.
The neural mobilization interventions were mostly passively induced by the therapist and included:
- Cervical lateral glides
- Upper limb sliders
- Upper limb tensioners
- A combination of upper limb sliders and tensioners
- Cervical lateral glides with upper limb sliders or tensioners
Most studies used neural mobilizations without or with minimal symptom reproduction. Two studies performed the neural mobilizations at the point of symptom reproduction, but in 14 studies, it was unclear whether or not symptoms were allowed to occur. The treatments had variable durations from as little as 1 week to 12 weeks. The number of treatment sessions per week ranged from two to seven sessions per week.
One study was classified as radiculopathy since its inclusion criteria required the presence of dermatomal numbness and/or myotome weakness. Fifteen studies were classified as the Wainner cluster, 4 were classified as the Hall and Elvey cluster, and 6 studies were classified as “other”.
Neural mobilizations versus no treatment
For the outcome pain, 3 high risk of bias studies were included, assessing 159 participants. The meta-analysis showed superior effectiveness for neural mobilizations in nerve-related cervicobrachial pain, both for the Wainner cluster and “other” subclassifications of patients, compared to no treatment. The pooled mean difference was -2.81, with the confidence interval ranging from -3.81 to -1.81, but the effect had high heterogeneity as the I-squared statistic was 79%. The magnitude of the effect was larger in the Wainner cluster subclassification.
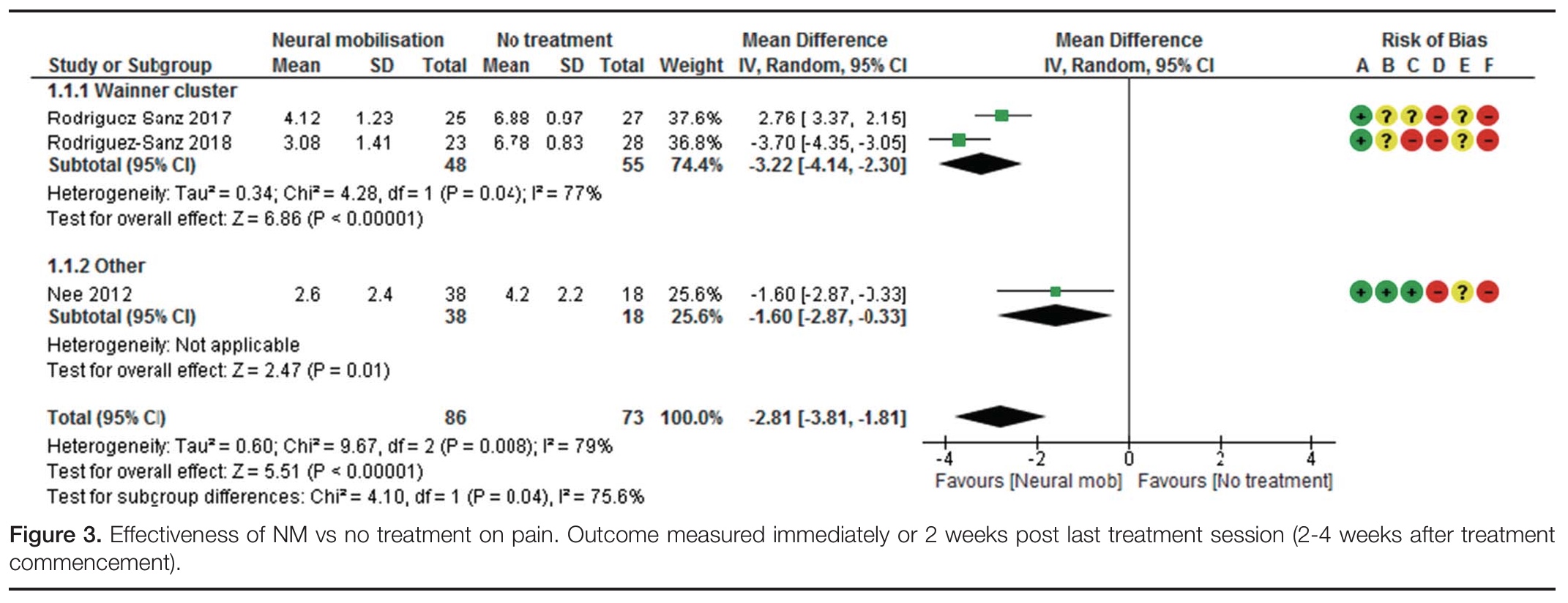
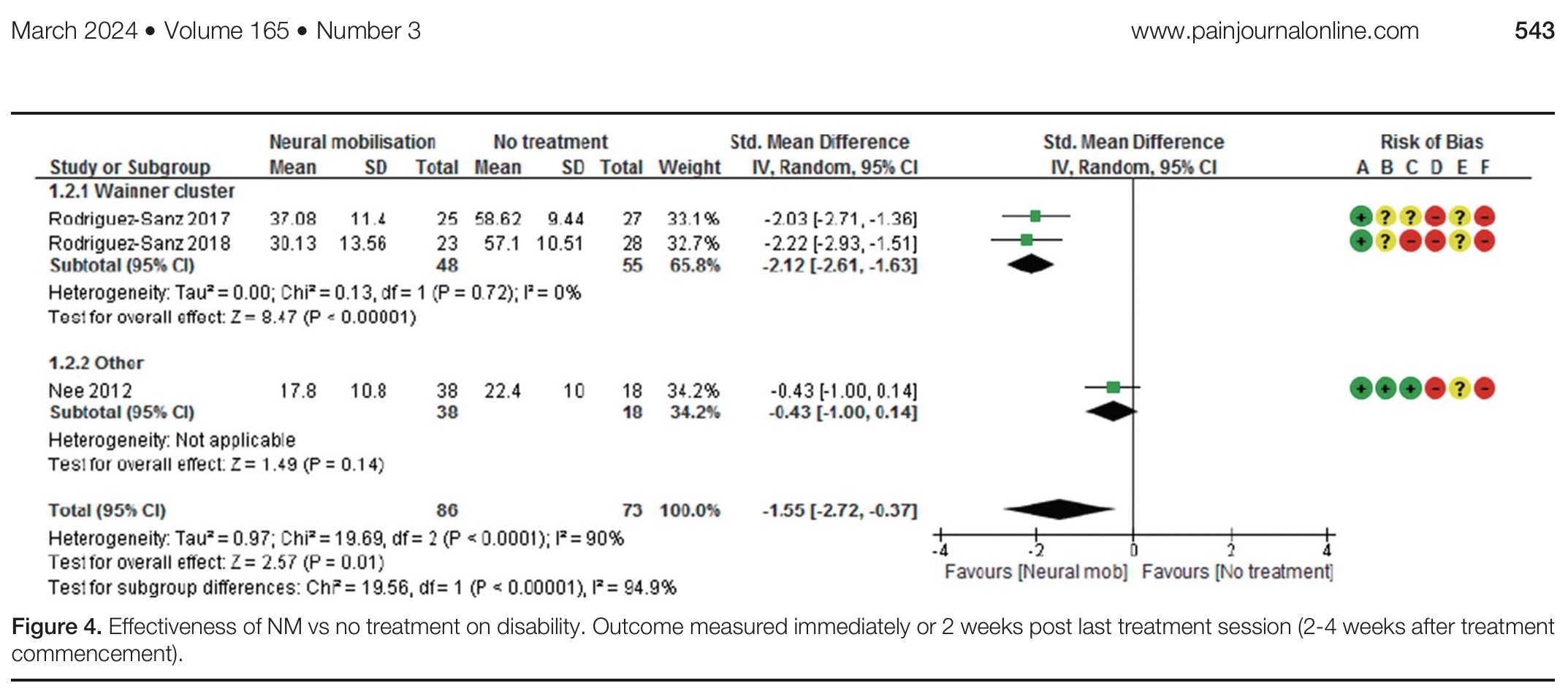
Three high-risk studies with 159 participants compared neural mobilizations versus no treatment for the outcome of disability reduction. The direction of the effect favored the neural mobilizations, with a mean difference of -1.55 and the 95% confidence interval ranging from -2.72 to -0.37. Here also substantial heterogeneity was also found by the I2 statistic. The Wainner cluster subclassification of patients had the largest effect, with no heterogeneity. No effect was shown in the study with the subclassification “other”.
Neural mobilizations versus cervical traction
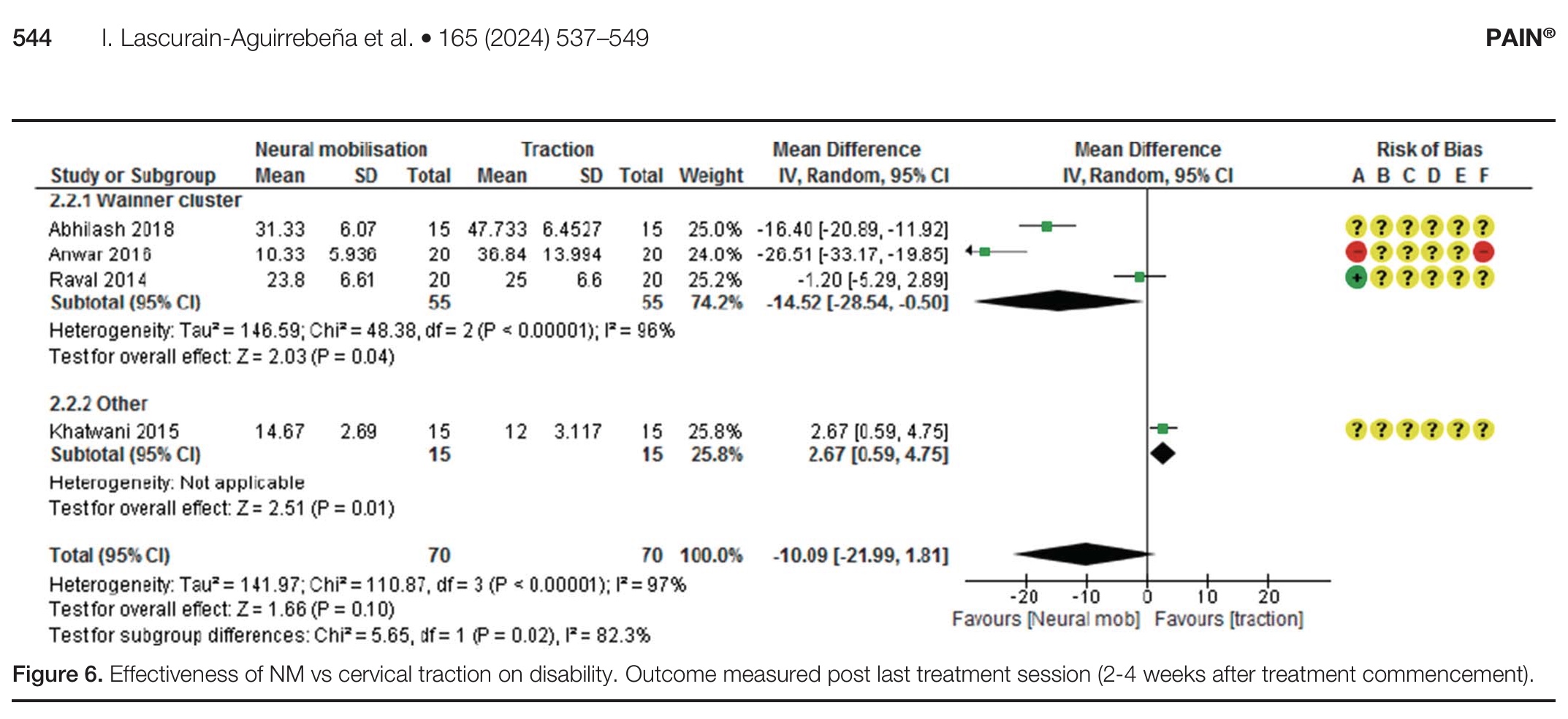
Considering the outcome of pain, four studies with 128 participants were included. No difference was found in the effectiveness of neural mobilizations versus traction, even after the removal of 2 high risk of bias studies in the sensitivity analysis. The subgroup analysis, however, found a significant beneficial effect favoring neural mobilizations in patients classified under the Wainner cluster. One study found traction to be more effective compared to neural mobilizations.
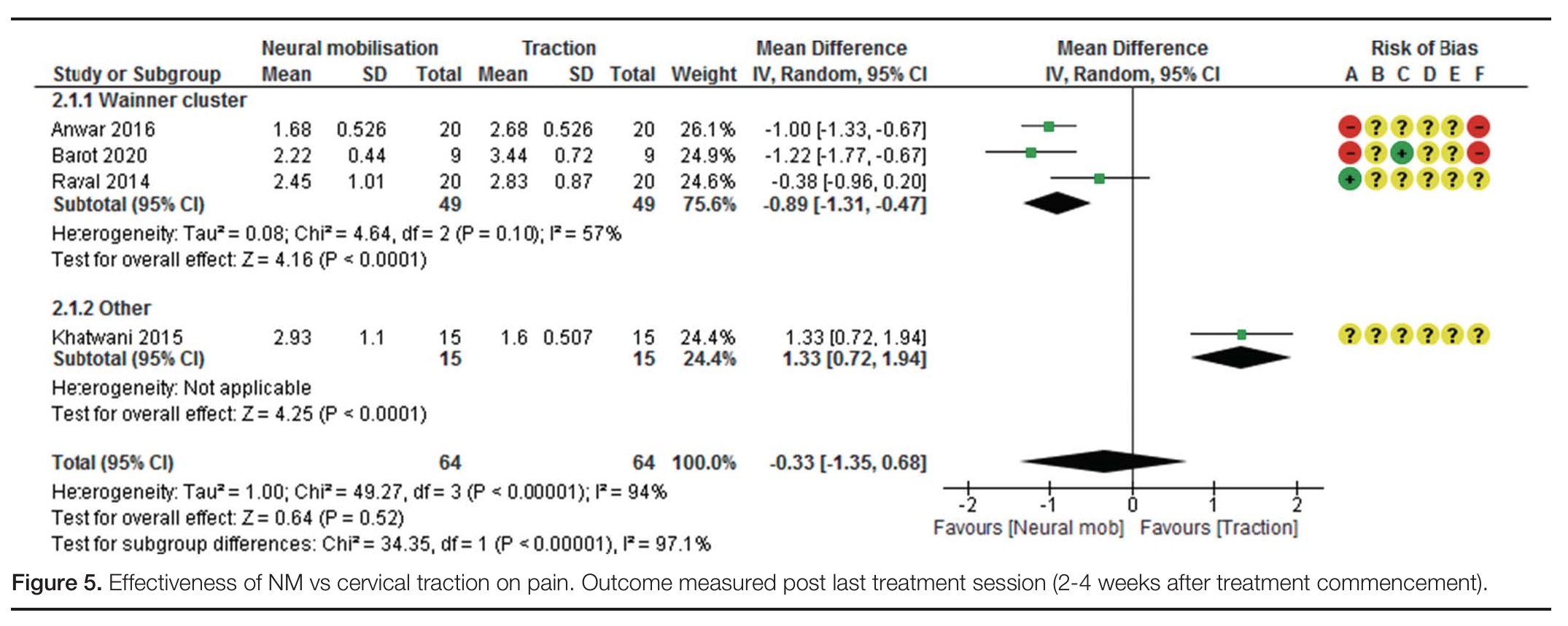
For the outcome of disability reduction, four studies with 140 participants were included. No overall difference was found between the two treatments, even after removing a high risk of bias study in the sensitivity analysis.
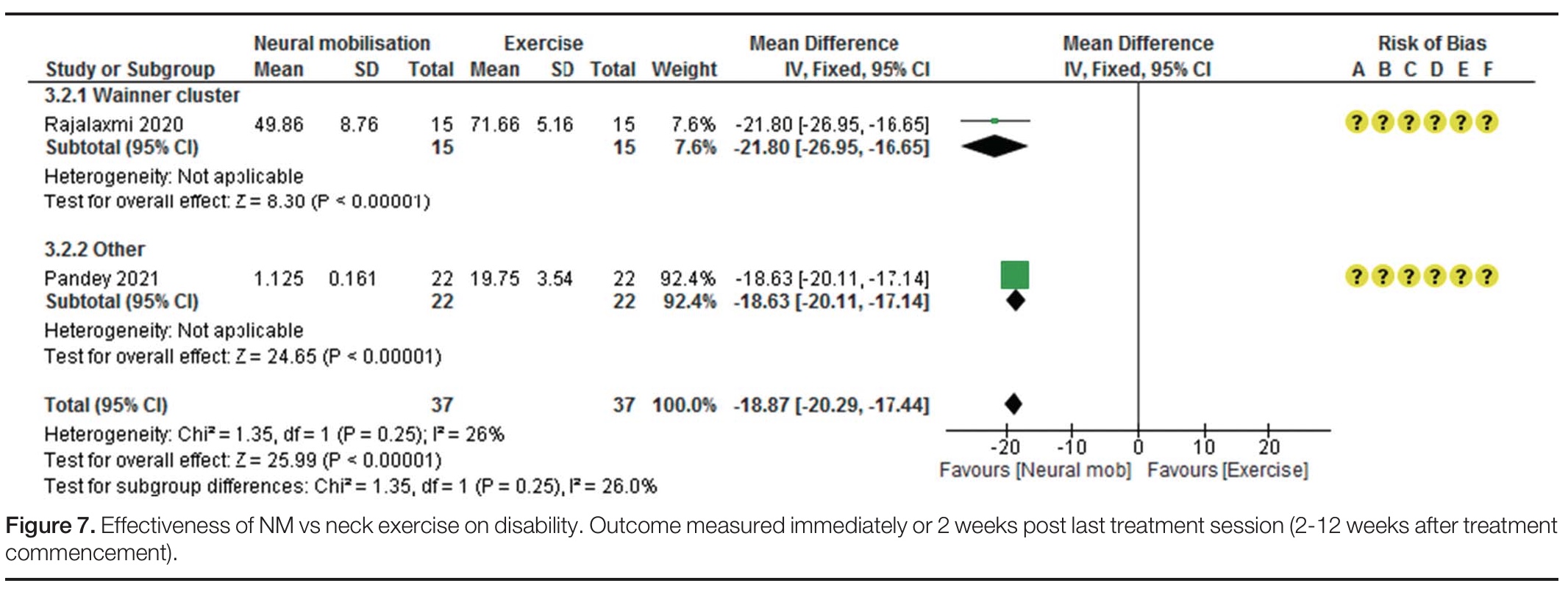
Neural mobilizations versus exercise
Two studies with 78 participants having nerve-related cervicobrachial pain were included, but no meta-analysis could be conducted regarding the outcome of pain. For the outcome of disability, two studies with 74 participants were meta-analyzed. The overall effect indicated that neural mobilizations were more effective compared to exercise for reducing disability in people with nerve-related cervicobrachial pain, with a mean difference of -18.87 and a confidence interval ranging from -20.29 to -17.44. Heterogeneity was low, as the I2 statistic was 26%. No differences were found between the patients classified as cervicobrachial pain according to the Wainner cluster criteria or other criteria. The GRADE rated the certainty of the evidence as moderate.
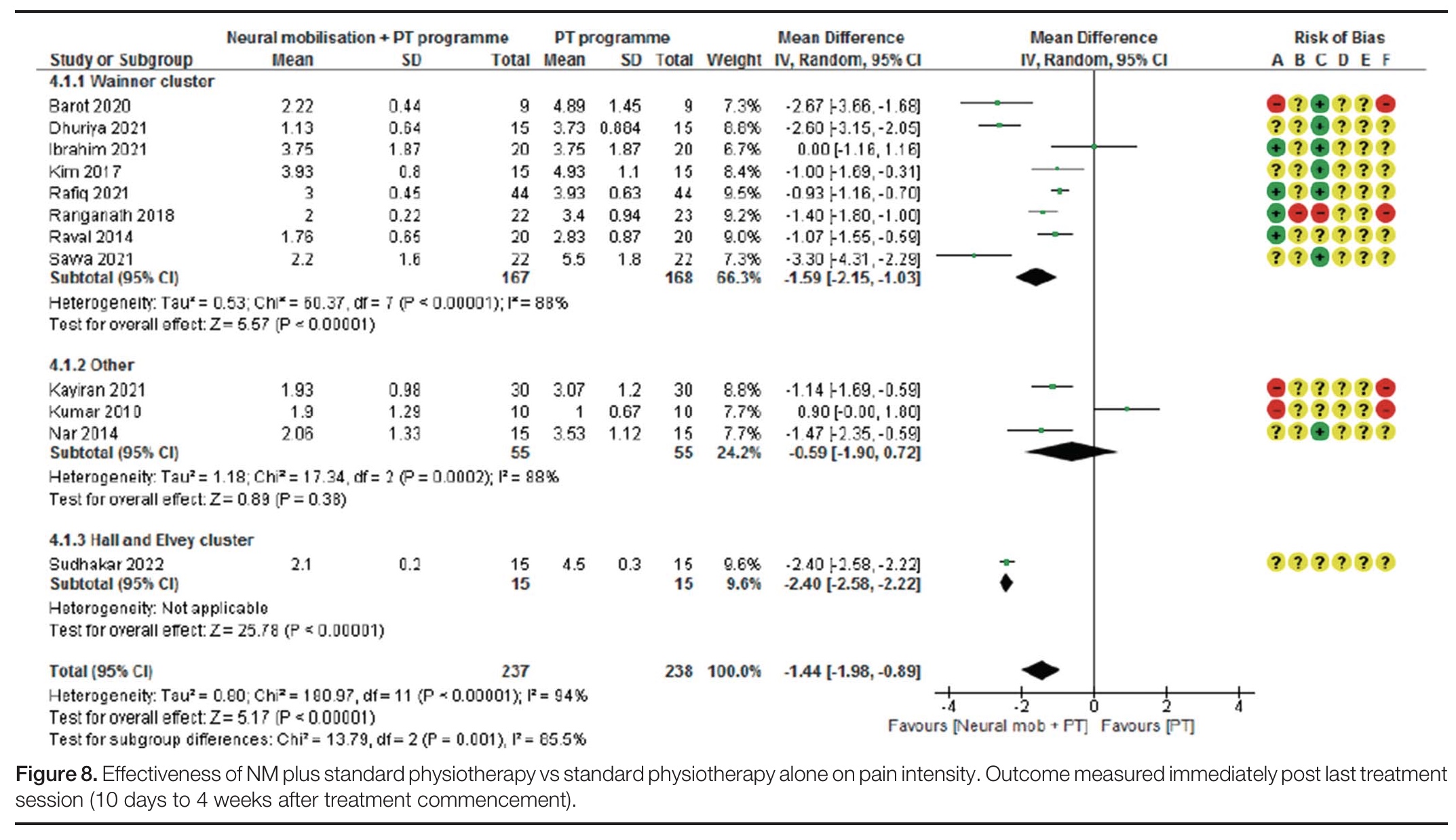
Neural mobilizations plus standard physiotherapy versus standard physiotherapy
Regarding the outcome of pain, twelve studies were included in the meta-analysis, covering 475 participants. For reducing disability, neural mobilizations were found to be more effective when added to standard physiotherapy compared to standard physiotherapy itself. The overall effect indicated a mean difference of -1.44, ranging from -1.98 to -0.89 in the 95% confidence interval. When four high risk of bias studies were removed, the effect remained significant in favor of the neural mobilizations. The largest effects of neural mobilizations for reducing pain were observed in the patients with nerve-related cervicobrachial pain classified as a positive Wainner cluster (8 studies) and in those classified with a positive Hall and Elvey cluster; however, the latter was derived from only 1 study. No effect was observed in patients classified with other criteria for nerve-related cervicobrachial pain.
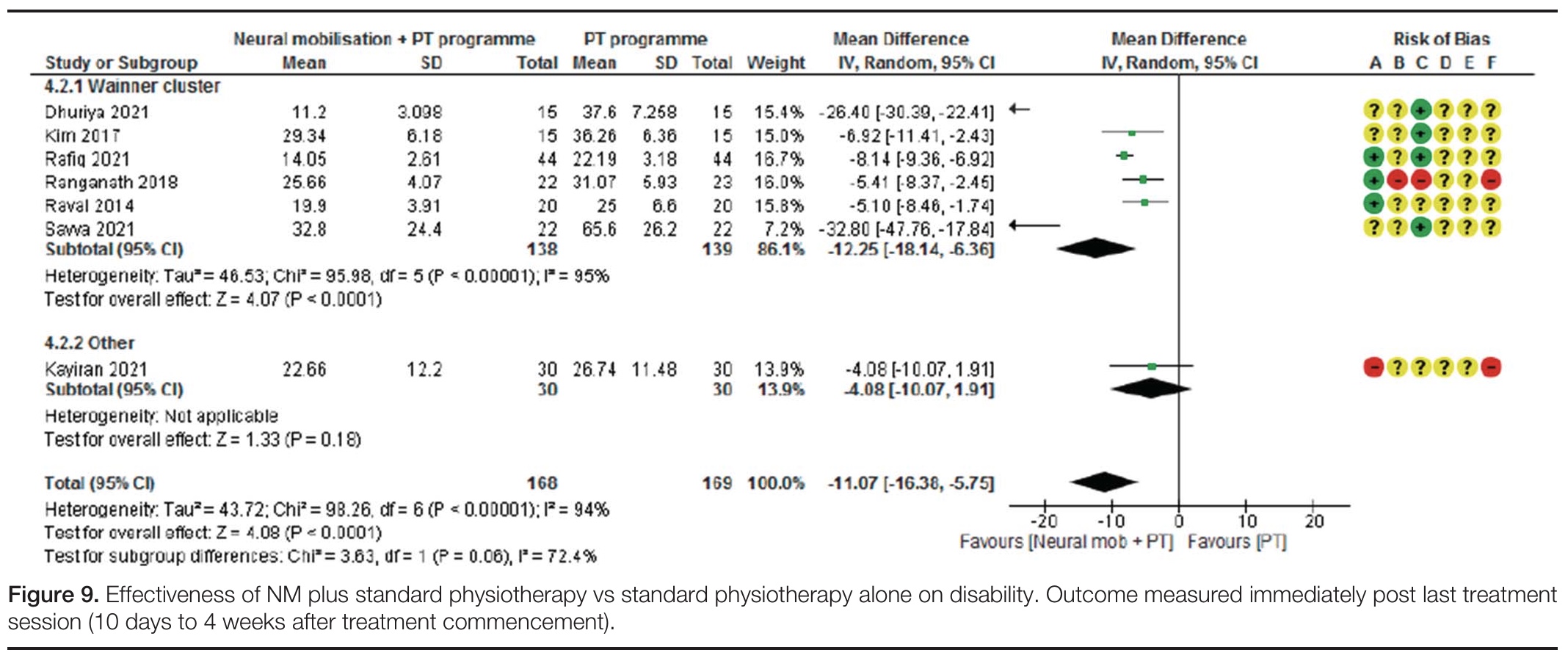
Concerning the outcome of disability, seven studies, including 337 participants, were meta-analyzed. Adjuvant neural mobilizations to standard physiotherapy were more effective than standard physiotherapy alone for disability reduction in people with nerve-related cervicobrachial pain. The mean difference was -11.07, and the 95% confidence interval ranged from -16.38 to -5.75. Differences remained significant even when two high risk of bias studies were removed in the sensitivity analysis. The effectiveness of adjuvant neural mobilizations added to standard physiotherapy was particularly seen in patients with nerve-related cervicobrachial pain identified by a positive Wainner cluster.
Neural mobilizations versus other modalities
No meta-analyses were possible since only one study each examined the comparison of neural mobilizations versus McKenzie manipulation/exercise, Maitland cervical mobilizations, ultrasound, laser, and oral ibuprofen, on the outcome of pain.
Even so, for the outcome disability, only one study each compared the effectiveness of neural mobilizations for reducing disability in nerve-related cervicobrachial pain compared to Mulligan cervical mobilizations, laser, and oral ibuprofen.
Questions and thoughts
Neural mobilizations were effective for reducing nerve-related cervicobrachial pain compared to no treatment, with a moderate effect. When added to “standard physiotherapy”, a moderate effect is observed, but the lower bound of the confidence interval is just below the MCID, indicating uncertainty about the meaningfulness of the latter comparison.
Regarding the outcome of disability, neural mobilizations were more effective compared to neck exercises, with a moderate effect. The confidence interval was narrow and ranged from a large effect to a moderate effect, indicating that the estimate is precise. When added to standard physiotherapy, neural mobilizations were more effective in reducing disability, but the lower bound of the confidence interval was below the MCID, indicating that for some patients with nerve-related cervicobrachial pain, no clinically meaningful effects are observed.
Most of the included studies compared the effectiveness of neural mobilizations as an adjunct to standard physiotherapy with standard physiotherapy alone. But what is defined as standard physiotherapy for nerve-related cervicobrachial pain? These studies varied a lot in their definition:
- Barot et al. (2020): interferential therapy plus deep cervical flexor exercises and isometric neck exercise in all directions, trapezius and serratus strengthening
- Dhuriya et al. (2021): intermittent cervical traction, cervical isometric exercises, scapular strengthening, levator and upper trapezius stretching
- Ibrahim et al. (2021): infrared radiation and traction
- Kim et al. (2017): cervical traction
- Rafiq et al. (2021): isometric neck strengthening
- Ranganath et al. (2018): mobilization with movement
- Raval et al. (2014): cervical traction
- Savva et al. (2021): cervical traction
- Kayiran et al. (2021): hotpack, TENS, ultrasound, lower and middle trapezius strengthening, stretching of upper extremity, isometric neck exercises, deep cervical flexor exercises, serratus anterior strengthening
- Kumar et al. (2010): “mackenzie manipulation”
- Sudhakar et al. (2022): hot pack, cervical lateral glide, and postural advice
As you can observe, the comparison of neural mobilizations versus standard physiotherapy included studies that utilized interventions which, based on current evidence, are not considered standard or effective treatments for this condition in many contemporary physiotherapy practices, like, for example, infrared radiation. Since some of these studies used interventions with limited or no evidence base, I assume that the conclusions might change if the comparator of standard physiotherapy were more in line with the modern, contemporary approach of our profession.
While some above-listed studies in this “standard physiotherapy” comparison only used cervical traction, the authors still included these in the comparison as being standard physiotherapy. This is odd since another meta-analysis (Figures 5 and 6) already covered neural mobilizations versus traction.
The effects of the neural mobilizations were more pronounced in patients classified under the Wainner cluster. While the Wainner cluster is designed to predict radiculopathy (which is characterized by objective signs of myotomal loss of strength and dermatomal sensory disturbances), this study did not include patients with objective motor and sensory conduction loss in this subgroup. In case true motor loss and sensory disturbances arose, patients were subgrouped under the term “radiculopathy”. Only when having a 3 out of 4 positive Wainner cluster tests, patients were grouped as such. Participants with increased neural mechanosensitivity, a local cervical dysfunction, and reduced active or passive cervical range of motion were grouped under the Hall and Elvey cluster. As you can see, 3 different patient subgroups may exist:
- Patients with true objective radiculopathy leading to a loss of function (motor, sensory)
- People with pain provocation from the Wainner cluster, indicating a gain in function (pain provocation) from nerve root sensitization
- People with more features of neural tissue sensitivity, whether this is due to a more central or peripheral sensitization
Although the Wainner cluster evaluates pain provocation manoeuvers (except for the traction test, which looks for pain reduction), the cluster was validated against EMG and MRI studies indicating a nerve root dysfunction due to radiculopathy. It may thus be possible that both clusters identify different patient populations.
Only one study included participants with true radiculopathy with a loss of function. As such, no evidence can be derived to support neural mobilizations in people with objective signs of radiculopathy. I would recommend that you use the Wainner cluster when you suspect your patient to be affected by radiculopathy, along with an objective neurological examination, including dermatomal and myotomal testing. If positive for the Wainner cluster but negative for the objective neurological testing, neural mobilizations will likely help reduce nerve root sensitization.
Talk nerdy to me
The majority of studies measured the effectiveness of neural mobilizations immediately following the last treatment session. Only three studies measured the effects one and two weeks following the last session. Therefore, evidence on the effectiveness of the neural mobilizations is mostly for the short term.
Considerable heterogeneity was observed in the effects, indicating a lot of variation between the studies. Variation can arise from multiple factors, like the specific patient population studied, the use of the techniques, the timing of the interventions, etc.
The effectiveness of neural mobilizations in nerve-related cervicobrachial pain may vary among different classification criteria (the patient subgroups in this study).
In 5 out of 7 meta-analyses, significant subgroup analyses were found, indicating that the classification criteria used play a significant role in the effectiveness of neural mobilizations for nerve-related cervicobrachial pain. When the Wainner cluster was used, 13 out of 14 studies indicated more favorable outcomes following neural mobilizations. Effect sizes were small (pain) to moderate (disability) when compared with traction, moderate (pain and disability) when compared with standard physiotherapy alone, and large when compared with no treatment (pain and disability) and exercise (disability). This altogether indicates the improved effectiveness of neural mobilizations in a certain subgroup of people with nerve-related cervicobrachial pain, scoring positive on the Wainner cluster.
Twelve studies were rated as having a high risk of bias, which is almost half of the included studies. Fifteen studies were rated as having “some concerns”. Publication bias was assessed through trial registries listing protocols from non-published studies, and found four registered but non-published trials. These authors were contacted, but no clear information was provided about the reasons for no publication. Systematic reviews and meta-analyses play a significant role in decision-making in modern evidence-based clinical practice. Meta-analyses pool data from all published RCTs. However, due to publication bias, the final analysis may lack negative evidence, which has either not been published or has been rejected, and this may impact the conclusions derived from the meta-analyses.
Take-home messages
- Neural Mobilisation vs. No Treatment: When comparing neural mobilizations to no treatment, neural mobilizations were found to be more effective at reducing both pain and disability. The effect size was large.
- Practical application: For patients with nerve-related cervicobrachial pain who might otherwise receive no intervention, neural mobilizations are a good starting point.
- Neural Mobilisation as an Adjuvant to Standard Physiotherapy: Adding neural mobilizations to standard physiotherapy increased its effectiveness for both pain and disability reduction. A moderate effect size was observed.
- Practical application: If you’re already providing standard physiotherapy, consider incorporating neural mobilization techniques. It appears to enhance the overall outcome.
- Neural Mobilisation vs. Exercise: For disability reduction, neural mobilizations were found to be more effective than exercise.
- Practical application: If exercise alone isn’t yielding sufficient results for disability, adding or prioritizing neural mobilizations may be beneficial.
- Neural Mobilisation vs. Cervical Traction: Interestingly, neural mobilizations were found to be no more effective than cervical traction for reducing both pain and disability.
- Practical application: This suggests that both interventions can be viable options, and your choice might depend on patient preference, availability of equipment, or your clinical reasoning for specific presentations.
Subgroup Differences are Key: The review consistently found that the effectiveness of neural mobilizations differed between patient subgroups:
- Wainner Cluster Patients: Neural mobilizations were consistently more effective than all alternative interventions (no treatment, traction, exercise, and standard physiotherapy alone) in patients who met the Wainner cluster criteria.
- Practical application: If your patient presents with nerve-related cervicobrachial pain and fulfills the Wainner cluster criteria, neural mobilizations should be a strong consideration in your treatment plan. The evidence suggests it’s particularly beneficial for this subgroup.
- “Other” Subgroup Patients: For patients classified as “other” (meaning they didn’t fit into the radiculopathy or Hall/Elvey clusters), the findings were less clear and varied. Neural mobilizations showed some benefit for pain but not disability when compared to no treatment, and no effect when added to standard physiotherapy.
- Practical application: For these patients, neural mobilizations might be less consistently effective, and you may need to explore other interventions or combinations.
- Radiculopathy (with conduction loss): The review highlighted that neural mobilizations were least effective in patients classified as radiculopathy (i.e., those with signs of conduction loss like dermatomal sensory loss, myotomal weakness, or hyporeflexia); however, this was based on only 1 study.
- Practical application: If your patient presents with clear neurological deficits indicative of radiculopathy, neural mobilizations might not be the most effective standalone treatment. Consider other modalities and focus on improving nerve function through other means.
While this meta-analysis provides valuable insights, it’s important to note that some included studies incorporated interventions, such as interferential therapy, hot packs, and ultrasound, which may not align with current evidence-based physiotherapy standards in many parts of the world. The presence of these studies, utilizing treatments with limited demonstrated effectiveness, likely contributes to the significant heterogeneity observed and warrants careful consideration when interpreting the overall findings. A focus on comparing neural mobilization with other established, evidence-based techniques in future research would be beneficial for advancing our understanding of optimal treatment approaches.
Reference
5 ESSENTIAL MOBILIZATION / MANIPULATION TECHNIQUES EVERY PHYSIO SHOULD MASTER
Learn 5 essential mobilization / manipulation techniques in 5 days that will skyrocket your manual therapy skills immediately – 100% For Free!