The Effect of Adding Mobilizations to an Exercise Program for Sacroiliac Joint Dysfunction

Introduction
Between 15-30% of patients with chronic low back pain have sacroiliac joint dysfunction syndrome (SIJDS). The pain can be present in the gluteal region, the lower back, abdomen, and even the entire lower extremity. The effectiveness of manipulations has been investigated and confirmed in previous studies and is, therefore, a recommended treatment. The literature is scarce on studies investigating manual therapy — that is, without manipulation. This study aims to investigate mobilization techniques added to a home exercise program for SIJDS.
Methods
Power was calculated a priori and the authors concluded that 64 participants would suffice, drop-out included. The inclusion criteria were:
- SIJ pain in the past month, VAS ≥ 3/10
- Between 18-60 of age
- SIJDS according to IASP guidelines:
- Pain around SIJ
- Positive on at least three of six validated provocation and motion palpation tests: distraction, compression, Gaenslen, posterior friction test, sacral thrust, and FABER tests
The exclusion criteria were:
- Underlying neuro deficits in leg
- Sacroiliitis
- Spondylolisthesis
- A prediagnosed disease of central or peripheral nervous system
- Current pregnancy
- Rheumatological disease
- Hx of major surgery of lower extremity and spine
Participants were divided into two groups:
Exercise group
Stretching: hamstring stretches, hip adductor stretch, piriformis stretch, quadriceps stretch, one knee to chest stretch, both knees to chest stretch, lower trunk rotation, and pelvic rotation stretch.
Strengthening: isometric hip abduction/adduction strengthening and prone position lumbar/hip-strengthening exercises were given as strengthening exercises
Programming for both stretching and strengthening: 2x/d, 5x/w, 3 weeks
Mobilization group
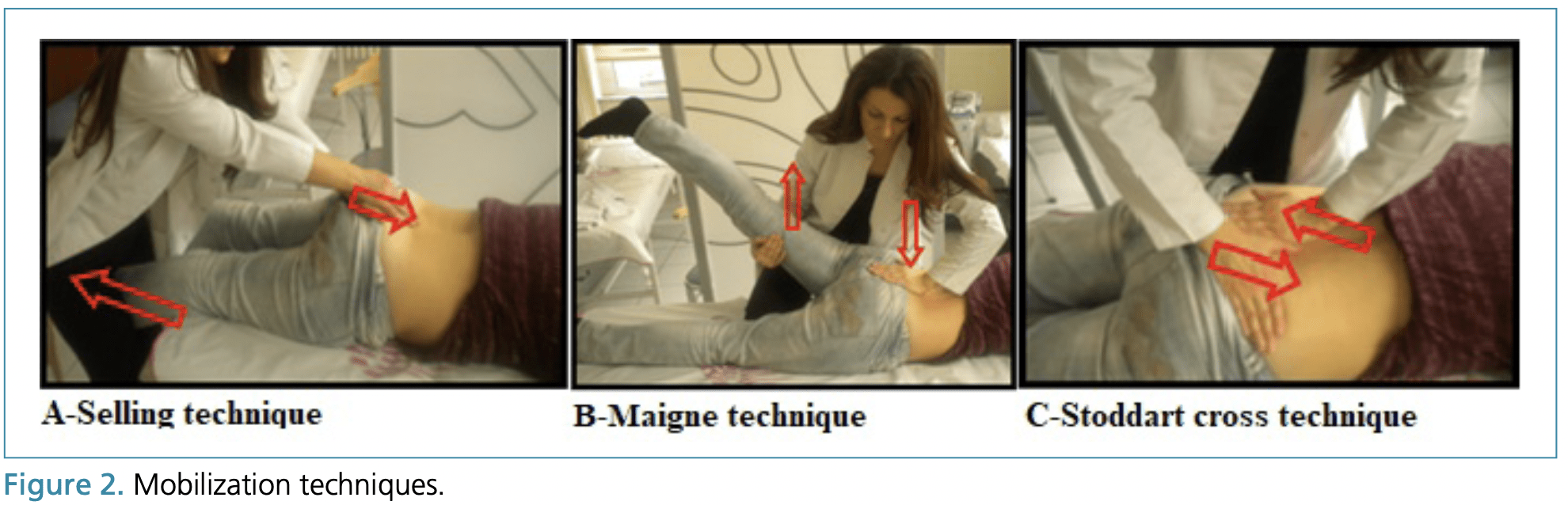
Mobilizations: anterior innominate, posterior innominate, Maigne technique, A-Selling technique, and Stoddart cross technique
Programming: 1x/w, 3 weeks
Results
The proportion of female patients was 61% and 75% in the exercise and mobilization groups, respectively. The mean age was 37 years and BMI was 24.
Both groups improved their VAS at one week and one month, compared to baseline. However, there were no between-group differences in any of the time points and variables.
Talk Nerdy to Me
Literature regarding the treatment of SIJD is scarce. Questions like the one that this trial asked need some answers. However, we cannot really answer the question that the authors proposed with this trial. That is because of several issues.
First of all, the trial was not registered. Although that is a pity, many authors don’t do this. A pre-trial registration lays out a plan that most often will be stuck to. This way, authors cannot swap outcome measures or analysis methods unnoticed to obtain a certain desired result.
An important aspect that they covered was power calculations. However, the research group did not specify which outcome measure they wanted to power, only an effect size. A power calculation is important since you want to minimize false negatives and indirectly false positives. No power means no useful study. Important to note is that this calculation speaks of one outcome measure, from a certain threshold (effect size 0.3 in this case), at a certain time point, with a certain analysis. Their power calculation showing adequate power for an effect size of 0.3 will in no way justify multiple measures at multiple time points.
Since we are talking about outcome measures, you probably noticed the lack of reporting in the methods section. None were given by the authors, and thus no primary outcome measure was specified. The authors did, of course, measure different parameters. They measured 19 variables per group in total, at three different time points. This does not work out mathematically as stated above. We would need an enormous study to be able to get useful information out of 19 variables.
The authors measure valid parameters such as the VAS in rest and activity, quality of life, etc. These are all important but futile because of the design. We cannot throw a bunch of variables at the wall to see which one sticks. There are a few measures that are distinct in my opinion. The authors measured the SIJ provocations again. The maneuvers are valid, this has been tested here (although recently this has been challenged as well). However, when the patient gets better but the thigh thrust test still hurts them, why should it matter? Certainly when keeping in mind that these kinds of tests have high false-positive rates.
Now, to the intervention. This study is in an ‘A vs A+B’ format. Usually, the group that receives the ‘+ B’ intervention (manual therapy), will do better. Not necessarily because of specific effects, but due to increased attention (non-specific effects, providers contact, face-validity, …). This was not the case. Can we explain that? Sure, the study was inadequately powered, possibly resulting in false-negative results. Another explanation is that the administered manual therapy provides no added benefits, however, this should be retested in a more robust study.
“But the patients got better, that means it works — right?” Not really. If you circle back to the inclusion criteria you can see that pain in the previous month was a criterium. That means that acute patients might roll into the study. This, in turn, means that natural history (or nature’s healing) can explain the results. This would have been fixed with a control group. However, the authors rightly note that this was not feasible due to ethical constraints (inviting someone to a study and not treating them sucks).
Let’s get into the intervention itself. The authors state that they gave out strengthening exercises to perform at home. The exercises were in no way strengthening. They might be called resistance exercises but not every exercise had resistance. So let’s just call them movements. If these movements might mediate any treatment effects is a discussion in and of itself. I’m sure different opinions exist. For this study, it does not even matter that much since both groups received them so the effects cancel each other out. We are interested in the effects of manual therapy in this study, although a statement about that cannot really be made due to the issues described above.
Take Home Messages
- We need more high-quality RCTs in the field of sacroiliac joint pain.
- Methods matter in RCTs.
- A home exercise program could work, but it might also be the natural history of the problem.
Reference
MASSIVELY IMPROVE YOUR KNOWLEDGE ABOUT LOW BACK PAIN FOR FREE
5 absolutely crucial lessons you won’t learn at university that will improve your care for patients with low back pain immediately without paying a single cent