Meniscus tear treatment - Surgery or exercise for Mechanical Symptoms?

Introduction
Adults receiving surgery for a meniscal tear frequently suffer clinical complaints and functional difficulties in their regular activities. Skou et al., in 2018 found that in young adults, mechanical symptoms were one of the most common patient-reported symptoms leading to surgery. Mechanical symptoms are symptoms of catching/locking or inability to extend the knee fully. The aim of this study was to compare early surgery to exercise and education for alleviating patient-reported mechanical meniscus tear symptoms. So which is better, surgery or exercise for meniscus tear treatment?
Methods
This RCT was a secondary analysis of the DREAM trial by Skou et al., in 2022. This original trial found that early meniscal surgery is not more beneficial to exercise and education than the option of later surgery among young, active adults with meniscal injuries. They found both groups had clinically significant improvements in pain, function, and quality of life at 12 months.
In the secondary analysis, we discuss here, the intent was to look in detail at the patients reporting mechanical meniscus tear symptoms. Can surgery or exercise help alleviate their catching, and locking symptoms, or improve full knee extension range of motion? What is the preferred meniscus tear treatment option for this subset of patients?
To answer this question, data from the DREAM trial was used. In brief, the original trial included 121 participants with MRI-verified meniscal tears between 18 and 40 years. They either received early surgery or were randomized to an exercise and education protocol. The exercise groups underwent a 12-week supervised program that included 60-90 minutes of neuromuscular and strengthening exercises performed twice per week. This was supplemented by two educational sessions, one at the beginning of the exercise program and one at the end.
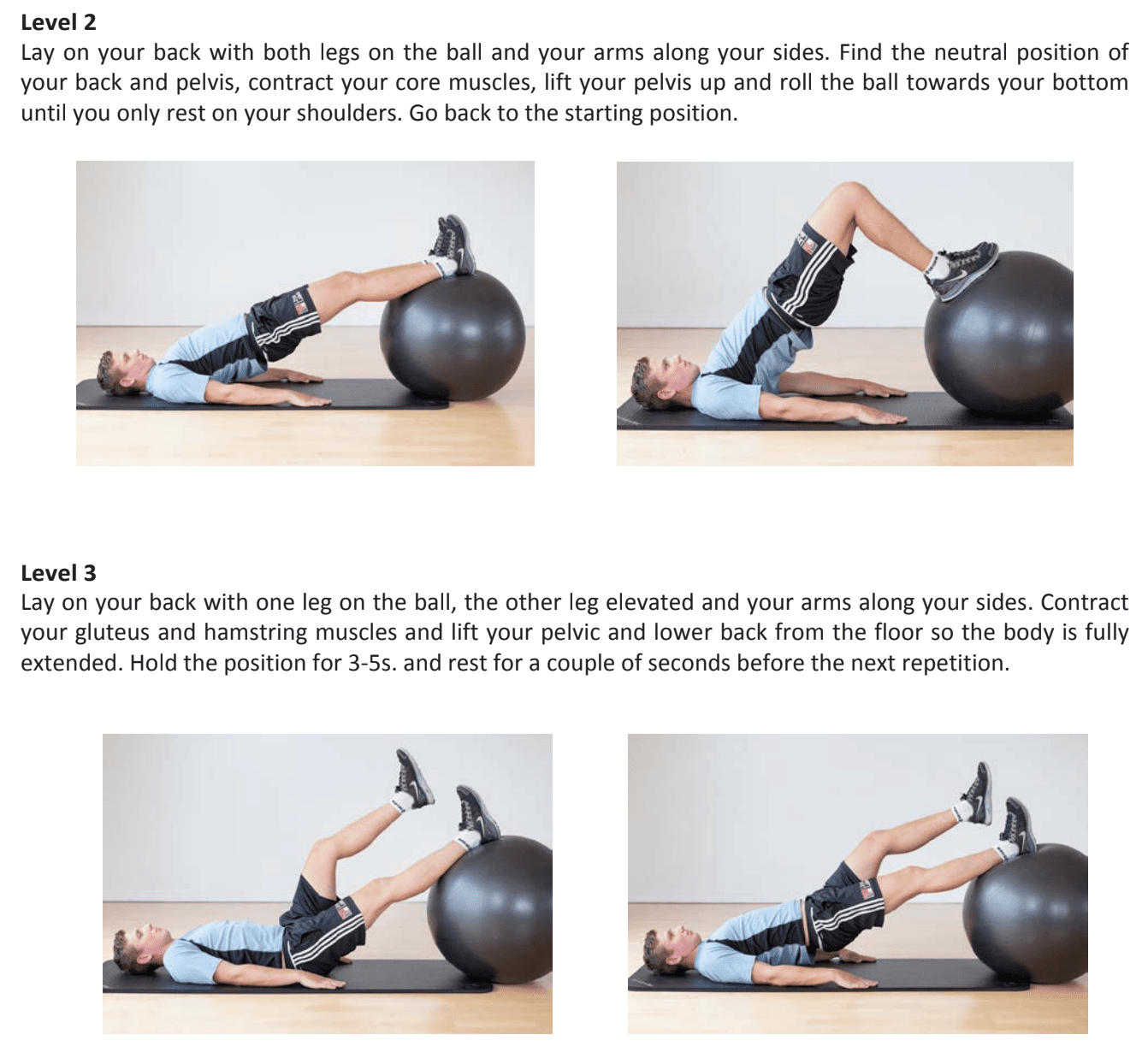
The program’s exercise sessions included a warm-up (5 minutes on a stationary bike), eight neuromuscular and four strengthening exercises focusing on the lower extremities, and a cool-down (5 minutes). Two additional exercises that concentrate on lowering swelling and enhancing range of motion were added if necessary. The neuromuscular exercises included knee bends, pelvic lift, plank, side plank, stair climbing, outer thigh and inner thigh exercises using an exercise band, slide-exercise sideways and sideway lunge and were individually fitted to each patient based on two to six levels of difficulty and performed in two to three sets of 10-15 repetitions. The strengthening exercises were a one-leg knee press, one-leg knee extension, one-leg knee flexion, and kettlebell swings.
In this secondary analysis, the main outcome was the presence versus absence of mechanical knee symptoms. This was assessed at 3, 6, and 12 months.
Results
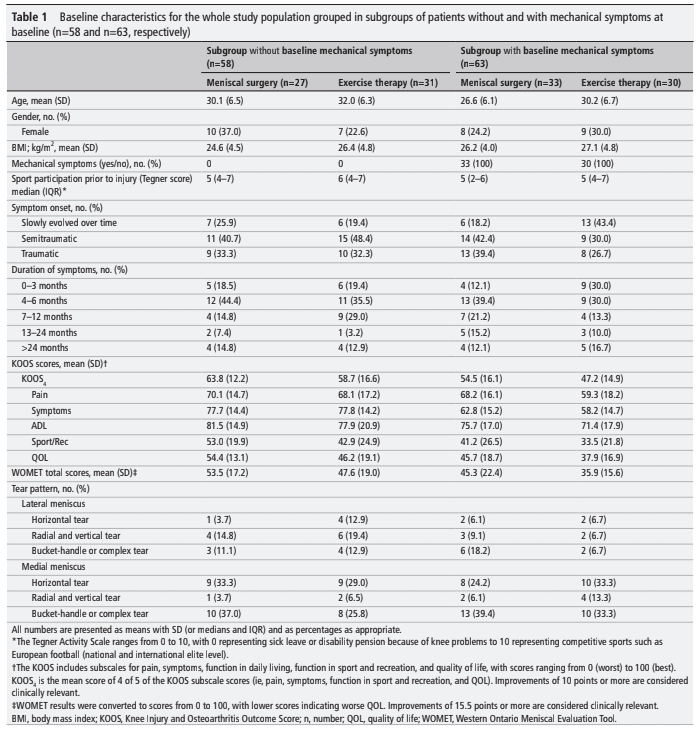
Only the participants who reported mechanical symptoms at baseline were included in this secondary analysis. Respectively 33 and 30 participants reported having these symptoms in the surgery and exercise groups,.
At the 12-month follow-up, 35% and 69% of the surgery group and exercise group respectively reported having mechanical meniscus tear symptoms. This leads to an odds ratio of 8.77 for a participant in the exercise group to report mechanical symptoms compared to a subject in the surgery group. The relative risk was 1.83 (95% CI 0.98 to 2.70).
Questions and thoughts
This analysis found that 69% of people reported having mechanical symptoms 12 months after participating in exercise as meniscus tear treatment. What stands out are the differences in the participants between both trial arms at baseline. For example, the symptom onset, duration of symptoms, and tear pattern. It is well understood that meniscus tear patterns can lead to different symptomatology. Also, a difference in the onset and duration of symptoms may give an indication of a heterogeneous study sample.
Further, the authors report variability in the presence or absence of mechanical symptoms over time. This confirms what was already found in the study by Sihvonen et al., 2016. Therefore it is recommended not to let this alone base someone’s decision on whether or not to opt for surgery. Rather, it is advised to monitor these symptoms over time before letting this guide the decision on whether or not to operate.
Talk nerdy to me
The results from this study came from a secondary analysis. It is important to remember that the study was not designed to answer this research question specifically. Therefore, This study may give insight into the relationship between mechanical symptoms and the interventions, but this should be tested further to draw firm conclusions. The limited sample size and the fact that a substantial number of participants had missing data on the mechanical symptoms at several time points and more in the surgery group may be limitations to this research.
Take home messages
The results of this study revealed that early surgery was more effective than exercise and education in reducing mechanical meniscus tear symptoms. However, this research was a secondary analysis from an earlier RCT which showed that early meniscal surgery was not more beneficial to exercise and education with optional delayed surgery among young, active adults with meniscal injuries. In the original RCT, both groups achieved clinically significant improvements in pain, function, and quality of life at 12 months. The current study, however, looked more closely in detail at the patients reporting mechanical symptoms to know whether they’d respond differently to these treatments. Here, it appears that in those with mechanical symptoms, surgery is better. When this is your patient’s main complaint, it could be interesting to refer to an orthopedic surgeon. When the patient has no mechanical symptoms, exercise combined with education could achieve the same results for pain, function, and quality of life compared to surgery.
Reference
Additional references
LEARN TO OPTIMIZE REHAB & RTS DECISION MAKING AFTER ACL RECONSTRUCTION
Sign up for this FREE webinar and top leading expert in ACL rehab Bart Dingenen will show you exactly how you can do better in ACL rehab and return to sport decision making



