Options for Improving Pain in Plantar Fasciopathy

Introduction
Unsatisfactory outcomes are achieved by many patients with plantar fasciopathy. As such, it remains a stubborn condition to treat. The condition primarily affects individuals in their twenties to sixties and this can limit one’s ability to participate in everyday work and activities. A recent systematic review concluded that no hard evidence exists on the preferred treatment of plantar fasciopathy. Although, it did not include heavy-slow resistance training (HSR), for which preliminary evidence suggests it is better than stretching the plantar fascia. As resistance training may take time, a corticosteroid injection is another option that can be offered to patients. The combination of both seemed feasible by an earlier pilot study by Riel et al., in 2019. Due to the lack of trials examining heavy-slow resistance training for plantar fasciopathy, this trial was held.
Methods
Eligible participants were recruited from general practices or from Facebook and suffered inferior heel pain of ≥30/100 VAS in the previous week, for at least 3 months, and had pain on palpation of the medial calcaneal tubercle or the proximal plantar fascia. The fasciopathy was confirmed using ultrasonography.
The effectiveness of three interventions were compared. Patient advice plus heel cup alone (PA) versus PA and lower limb exercise (PAX) versus PAX plus corticosteroid injection (PAXI).
Every group received information about plantar fasciopathy and a heel cup. The advice was given both verbally and through a leaflet and included information about the pathology, risk factors, and load management. The heel cup was made from silicone, but were allowed to wear their own foot orthoses if they preferred them above the heel cup.
The PAX and PAXI groups also performed heavy-slow resistance training exercises on top of the advice and wearing the heel cup. They performed a toe-elevated heel raise on a step, consistent with the 2015 Rathleff trial. The load was as heavy as possible, but participants had to make sure to achieve 8RM maximum. The exercise could be performed bilaterally, but when this was insufficient to achieve an 8RM, the exercise was done on one leg or loaded with weights or backpacks. Tolerable pain during the exercise was allowed and participants were instructed to perform the exercise every other day until symptoms reached a self-evaluated satisfactory result and then for an additional 4 weeks.
Participants randomized to the PAXI group followed the same protocol as the PAX group, but they were not allowed to add load to achieve an 8RM until the third week after the injection. The injection was guided by ultrasound and inserted in the deep and superficial plantar fascia.
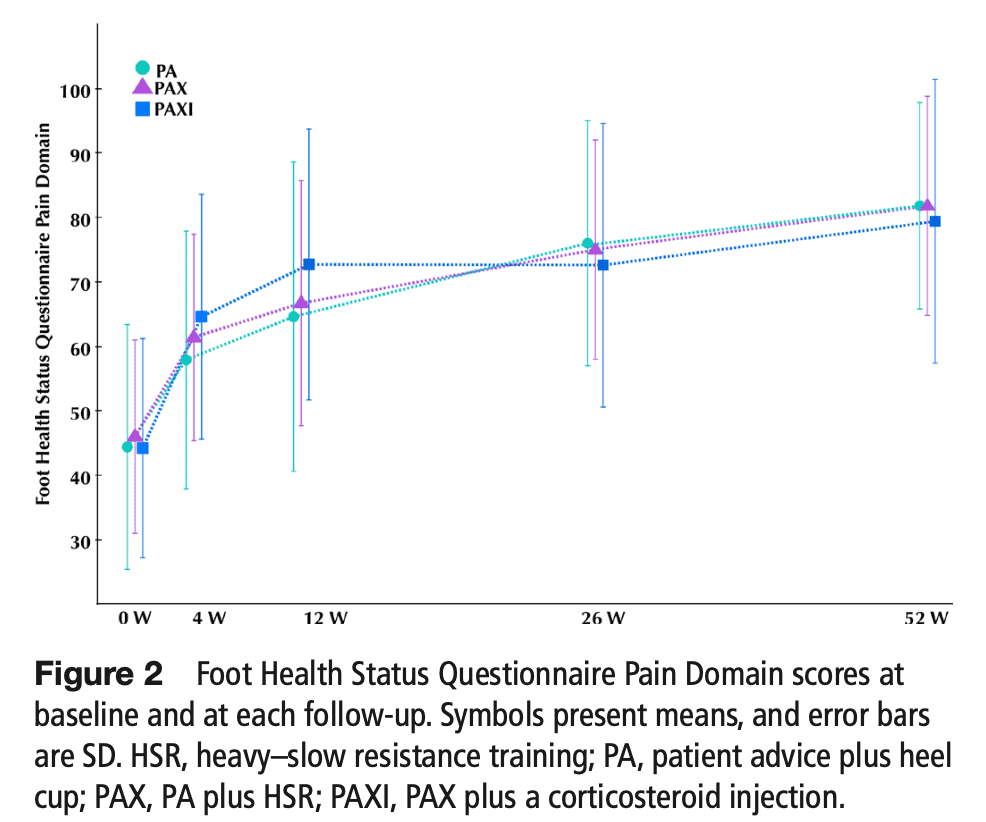
The primary outcome of interest was the 12-week change in self-reported pain, measured from the pain domain of the Foot Health Status Questionnaire (FHSQ). This questionnaire ranges from 0, representing worst, to 100 which equals best. The minimal important difference in the pain scale of this questionnaire is 14.1 points.
Results
Hundred-eighty people with plantar fasciopathy were included in this randomized controlled trial. They were comparable at baseline. When looking at the primary endpoint at the 12-week follow-up, the analysis revealed a statistically significant difference in self-reported pain between the PA and PAXI groups, which favored PAXI (adjusted mean difference: −9.1 (95% CI −16.8 to −1.3; p=0.023)). This significant difference was maintained at the 1-year follow-up (adjusted mean difference: −5.2 (95% CI −10.4 to −0.1; p=0.045)).
Questions and thoughts
The results from this trial indicate that patient advice combined with a heel cup, heavy-slow resistance exercise, and a corticosteroid injection was statistically better than patient advice plus a heel cup alone. However, being statistically significant, the mean difference did not surpass the MCID of 14.1 points, thus questioning the relevance. This means that up to now, we cannot say that one treatment is superior to the other. As such, we can offer many valid options, and try to match these to the patient’s preferences.
The primary endpoint was set at 12 weeks. This may seem long for participants who are in pain but seemed short to me especially as the trial compares a corticosteroid injection that is expected to give short-term benefit to a resistance training protocol which may need time for leading to improvements. Nearly every trial comparing injection to exercise find short-term benefits favoring injections, while we know that exercise requires more time to lead to good outcomes. Here, the 12-week analysis did not favor one treatment over another and therefore we shouldn’t worry about this. But, I think we should ask ourselves if we can really compare exercise and injection in the short term. Personally, I think that 8-12 weeks is short to compare findings between these two different interventions. For example, Brown et al., in 2017 provided a case report of 8 weeks of intense strength training with two active, male participants. Here, the maximum voluntary contraction showed only a little increase compared to the baseline at 8 weeks. So if a strengthening intervention is given with the aim to reinforce the foot and thereby reduce pain, we cannot compare the effect in pain reduction when no strength increase has occurred yet. Therefore, in my opinion, we cannot compare the effects of injections that were shown effective for many conditions in the short term with exercise needing more time to lead to improvements.
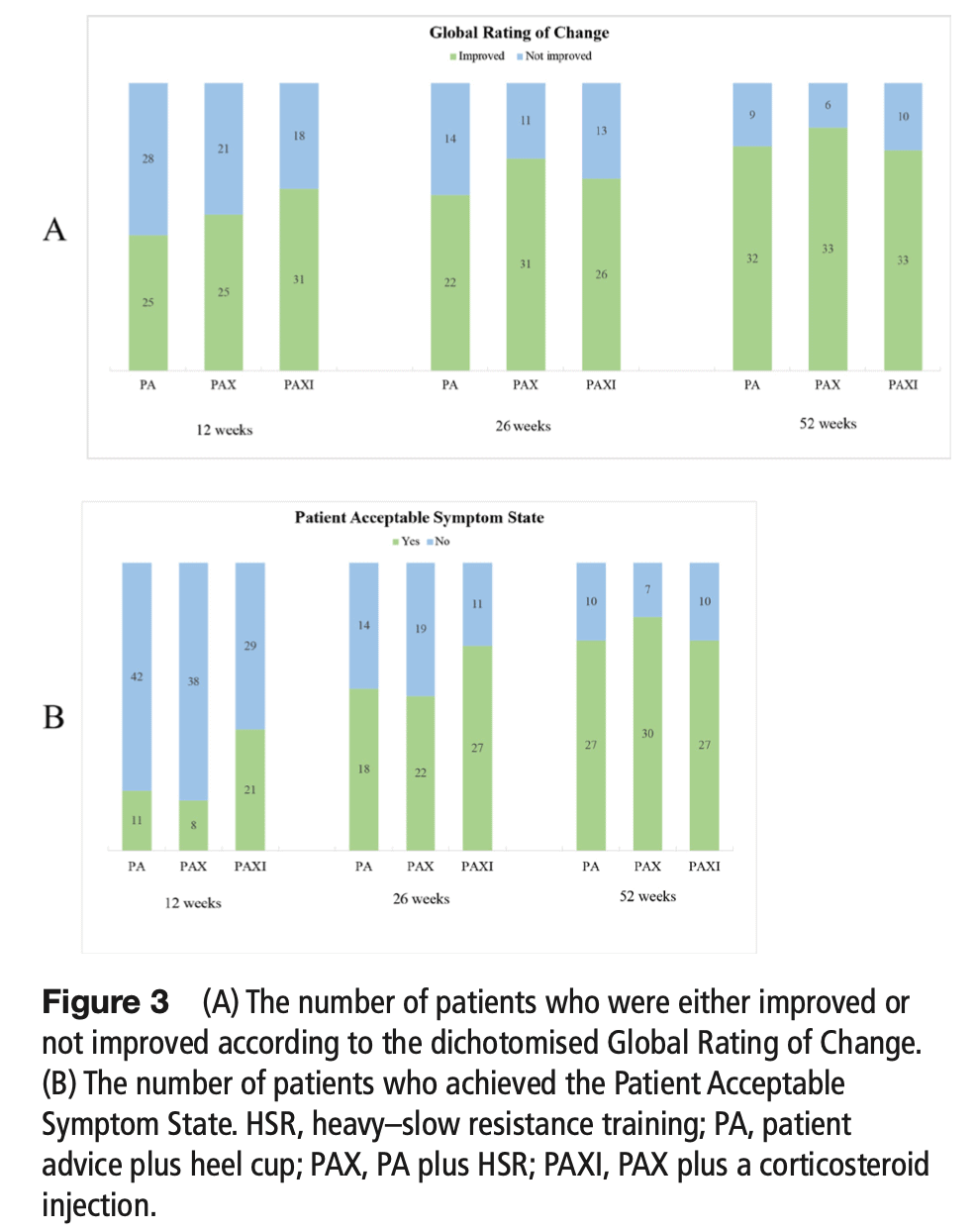
Of course, people in pain may prefer the “quick fix” and therefore we can assume someone would rather choose the injection. Yet, the qualitative analysis revealed many different opinions from patients with plantar fasciopathy on their preferred treatment option. Six participants were interviewed after they ended the trial and were presented with the group results of the 12-week follow-up. They were asked which treatment they would recommend to a friend with plantar fasciopathy. Five of them said they’d recommend heavy-slow resistance training, four indicated they’d recommend a corticosteroid injection but not as a first-line option, and two of them would recommend the use of better shoes.
The participants agreed that conducting heavy-slow resistance exercises was appropriate because they considered it as a minor investment to make for the chance of a change, despite the fact that they were in so much pain that any improvement would be welcome. When participants were presented with the long-term outcomes at 26 and 52 weeks, only two of them would advise the use of corticosteroid injection, and this was reliant on high pain intensity and a strong desire for acute pain relief. Two would choose heavy-slow resistance training as their preferred treatment. Four participants stated that the choice of treatment was unimportant when the long-term outcomes were the same, implying that treatment is unnecessary if those suffering from plantar fasciopathy are patient enough.
Talk nerdy to me
Most trials on corticosteroid injections find improvements up to 6-8 weeks after the injection but not beyond that time. In this study, improvements were seen from 4 weeks already to 12 weeks. The authors suggest that this may reflect the effect of combining the strengthening program with the corticosteroid injection.
Three patients responded to the interviews that performing heavy-slow resistance training would only need to improve FHSQ pain scores by 2 points, which was the difference between PA and PAX at 12 weeks in the mean group comparison, one participant responded that it would need to improve FHSQ pain scores by 10 points, and one participant responded that it would only need to improve FHSQ pain scores by a few points. The MCID in the FHSQ pain was reported to be 14.1 points. But here the authors indicated that the MCID was calculated in a different environment and among Australians using the FHSQ and Global Rating of Change score, which allow participants to score their current symptoms and how much they have improved since the beginning of the treatment. GROC use has come under fire for generating recall bias. The MCID could be further tested in upcoming studies.
Take home messages
At twelve weeks, the PAXI group was statistically significantly better than those receiving advice and a heel cup and than those combining advice, a heel cup, and heavy-slow resistance training. Yet, the between-group difference did not surpass the MCID. This means that no intervention was proven superior over the other. At 26 and 52 weeks, the scores over the intervention groups were comparable. This indicates that time may be an important factor in the recovery from plantar fasciopathy.
Reference
Additional reference
DISCOVER FASCIA FROM ITS HISTORY TO ITS VARIOUS FUNCTIONS
Enjoy this free 3x 10min Video Series with Renowned Anatomist Karl Jacobs who will take you on a trip into the world of Fascia



