Immediate response to injection in subacromial shoulder pain

Introduction
Determining what treatment to offer someone with subacromial shoulder pain may be challenging as many reasons can elicit this pain. Treatment options available are injection, exercise, and surgery and they are all supported by low to moderate effect sizes. In the NHS, corticosteroid injection combined with best practice advice from a physiotherapist was found to be the most cost-effective option. In most cases, surgery is not needed or can be avoided. However, it remains challenging to determine which care path someone with subacromial pain should follow. Most of the time, a 6-12 week conservative approach with physiotherapy is initiated. This is however a relatively long period for those who are unlikely to respond to conservative care. It was reported that 77% of British Elbow and Shoulder Surgery Society members consider a good response to subacromial injection to be the best predictor of good surgical outcomes. But to avoid this waiting period, this study tried to provide an accurate differentiation between those in need of surgical intervention much earlier, based on the immediate response to injection in subacromial shoulder pain.
Methods
A prospective cohort study was set up to study the association between immediate response to injection and non-surgical care outcomes at 12 weeks post-injection in those with subacromial shoulder pain.
Adults referred to the orthopedic department for a new episode of subacromial shoulder pain received a corticosteroid injection and local anesthetic to the subacromial space. This was followed by a physiotherapy appointment one week following the injection. The post-injection physiotherapy visits were pragmatically delivered with the interventions and the total number of visits at the discretion of the physiotherapist.
The SPADI questionnaire was filled at baseline, and at 6 and 12 weeks following the injection. The percent change in SPADI from baseline was chosen as the primary outcome measure of this study. Each score out of 130 was converted to a percent. To obtain the percent change score from baseline, the following formula can be used: SPADI (% change) = (Follow-up (%) – Baseline (%)/Baseline (%)) x 100.
Other outcomes were the post-injection change. This was rated during active elevation of the arm in the scapular plane. Three attempts were performed. The participants received the instruction “take your arm up as far as you feel you are able”. Two points were recorded: P1 which was the ROM at pain onset, and P2 which was the maximal ROM. Worst and average pain during these 2 movements were recorded on a 100mm visual analog scale. Interestingly, these measurements were obtained 20 minutes before the injection and 20 minutes after the injection.
Results
A total of 64 adults were referred to the orthopedic department by their GP’s. Their baseline findings are displayed in the table below.
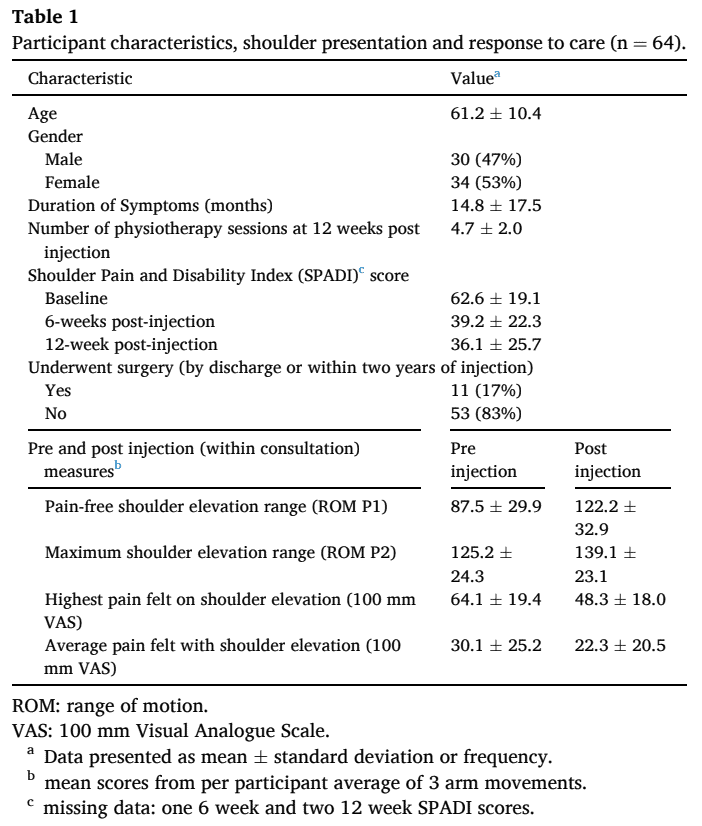
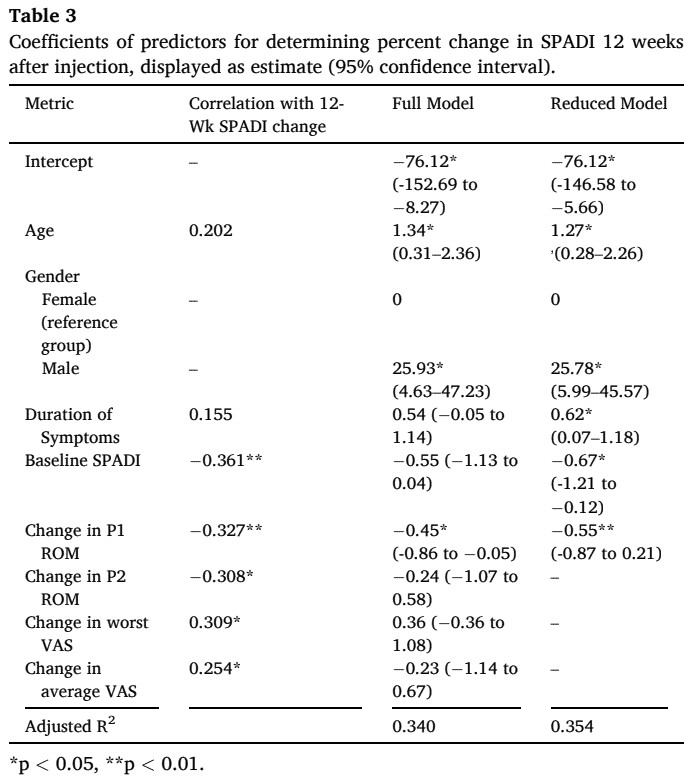
Their mean SPADI scores improved from 62.6 +/- 19.1 to 36.1 +/- 25.7 after 12 weeks post-injection. After 6 weeks post-injection, the change in P2 ROM was the only significant predictor of the percent change in SPADI. The predictors for a better 12-week percent change in SPADI were:
- Post-injection improvement in pain-free ROM (P1 point)
- Higher baseline symptoms
On the other hand, predictors for worse SPADI outcomes twelve weeks post-injection were
- Longer symptom duration
- Higher age
Questions and thoughts
The study found that increased shoulder elevation immediately after the injection was a prognostic factor for better outcomes after conservative care. This is interesting because, as mentioned earlier, 77% of British Elbow and Shoulder Surgeons consider a good response to injection to be a good predictor of satisfaction with surgery. Rather than being solely a treatment option, a subacromial corticosteroid injection can thus have prognostic value. But it doesn’t give you THE answer. It can be prognostic of good outcomes after both conservative and surgical management. Noteworthy, the statement that surgeons consider the response to injection prognostic for good surgical outcomes came from an expert consensus paper.
This result can probably be extrapolated to other paths of care. I assume that when you encounter someone with high levels of pain and you manage to increase their pain-free ROM, you can probably expect similar outcomes. Of course, having high initial pain scores can lead to regression to the mean. According to Barnett et al. (2005), the effect of regression to the mean in a sample becomes more noticeable with increasing measurement error. Here we should point to the standard error of the goniometer measurements of arm ROM used in this study. The authors reported a standard error of 17°. This means that to obtain a true change in ROM, an increase of more than 17° should be observed post-injection in each individual to be sure that this increase reflects a true change.
Talk nerdy to me
This observational study proposes the existence of 3 groups of patients:
- Those with immediate good response to injection who do well in the long-term with post-injection physiotherapy
- Those with only an initial good response, but who do not respond well to post-injection physiotherapy
- Those who do not obtain a good post-injection response
According to the authors, people with a good immediate response to injection in subacromial shoulder pain (those in the first group) can be managed conservatively with physiotherapy. Especially when they are younger, female and have more acute symptomatology. Those in groups 2 and 3 are thought to benefit more from surgery. However, this study had a sample of 64 adults, of whom only 11 progressed to surgery within 2 years post-injection. This is a low conversion rate and this was not the primary objective of this study. With the follow-up of only 12 weeks, the results cannot be generalized to longer term outcomes. Important to consider as well, is the observational design, which limits us to determine cause and effect. The authors have tried to explain variability in the SPADI outcomes. The model studied here explained 35% of the SPADI score at 12 weeks. Only 11.6% of the 12-week SPADI score was explained by the increase in pain-free ROM post-injection. This means that a lot of other factors have caused the SPADI to improve. Of note, at 6 weeks the only significant predictor for percent SPADI change was the change in maximal ROM.
It appears that shoulder function and disability improve gradually. It appears that first, maximal ROM is improved, and this is followed by improvements in pain-free ROM. Confounding factors like age, gender, baseline SPADI and duration of symptoms were also found to be significant predictors of the change in SPADI at 12 weeks.
Take home messages
People with a good immediate response to injection in subacromial shoulder pain are more likely to obtain better outcomes in shoulder pain and disability after 12 weeks. The increase in pain-free ROM immediately after and higher symptomatology are predictors of a better outcome in SPADI at twelve weeks.
Reference
LEARN TO DISTINGUISH SHOULDER FACTS FROM FICTION
Awarded World Leading Shoulder Expert Filip Struyf takes you on a 5-Day Video Course to Bust Lots of Shoulder Myths that Prevent you From Delivering the Best Care for your patients with Shoulder Pain



