Hip strength after ACL reconstruction

Introduction
A side effect of ACL ruptures is the risk of developing early-onset osteoarthritis (OA). Webster and Hewett found no difference in this risk when different management strategies were used to treat the ACL tear. It is thought that increased forces on the knee due to muscle imbalances and/or weaknesses may have a spell on it. Quadriceps weakness is considered the main driver for OA onset and progression. Less is known about the influence of hip muscle strength on the progressions of OA. Rotational strength was of particular interest in this study as it is thought to influence knee positions in the frontal plane (varus/valgus). As such, hip strength after ACL reconstruction was studied and if it was associated with symptoms, performance, and structural changes in cartilage outcomes.
Methods
The data from this study were obtained from a cohort study by Culvenor et al. 2015 who determined the factors associated with knee OA in subjects who underwent ACL reconstruction. They found an increased risk in the ACL reconstructed knees, compared to the contralateral healthy knee. The patellofemoral joint was particularly affected after ACL reconstruction. Hence why this study was interested in the rotational strength of the hip muscles, as this can influence varus and valgus around the knee and subsequently patellofemoral joint stress.
Hip rotation strength was assessed using a hand-held dynamometer one year after the ACL reconstruction. The assessment was done with the patient in the prone position and the hip in neutral and the knee flexed to 90°. Strength was assessed 3 times and the peak value was obtained for each limb. These values were multiplied by the lever arm and normalized to body weight.
Further, functional performance was assessed using the single hop for distance, triple crossover hop, side-hop, and one-leg rise.
At 1 and 5 years post-ACL reconstruction, participants filled in the Knee Injury and Osteoarthritis Outcome Score (KOOS). The KOOS-Patellofemoral (KOOS-PF) subscale was also obtained. They also obtained MRI scans that described cartilage defects in the patellofemoral and tibiofemoral compartments.
Results
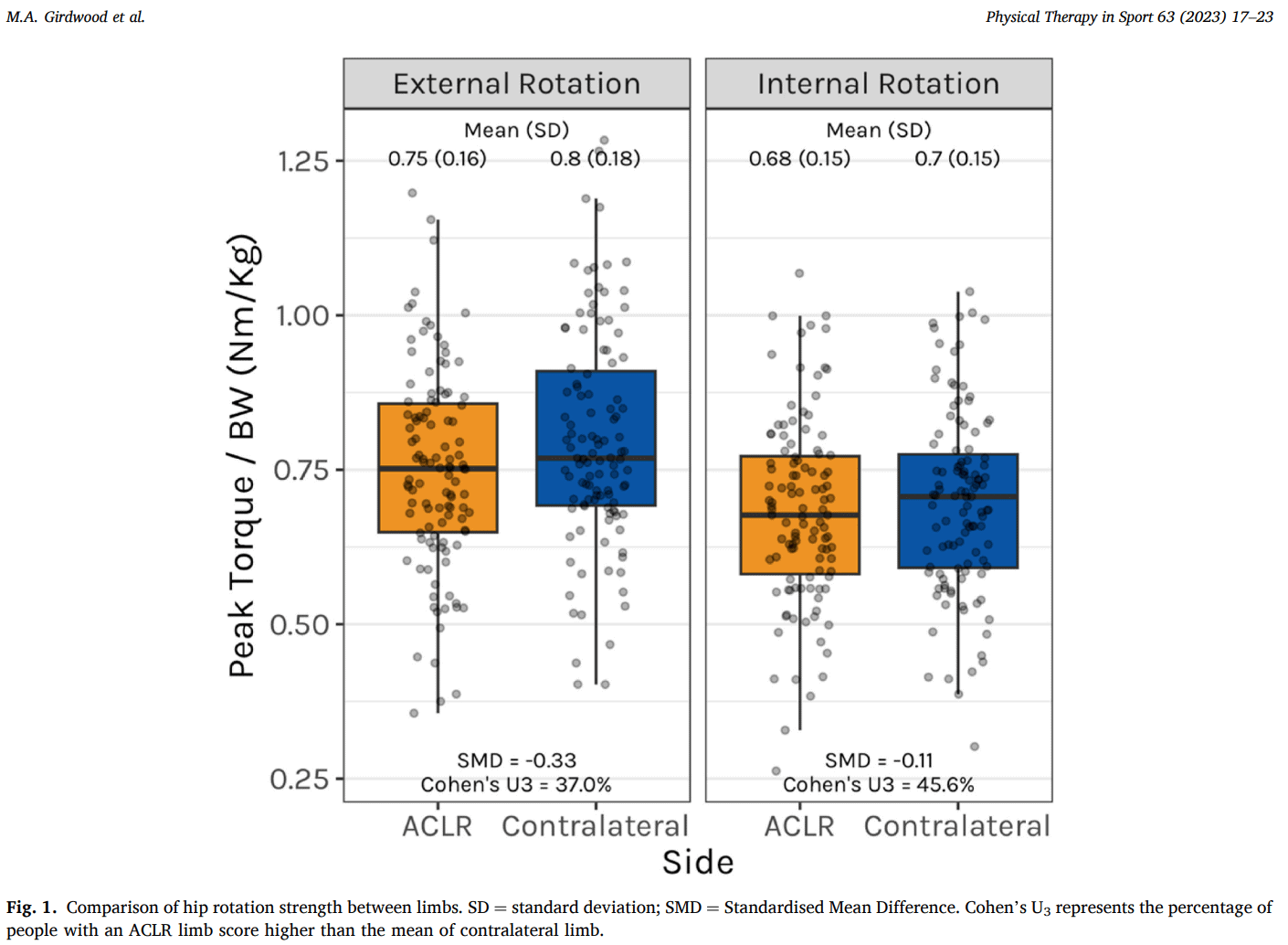
A total number of 111 participants completed the baseline examinations and 74 of them completed the 5-year follow-up. A small difference of 0.05 Nm/kg in hip external rotation strength was found between the ACL-reconstructed limb and the contralateral limb.
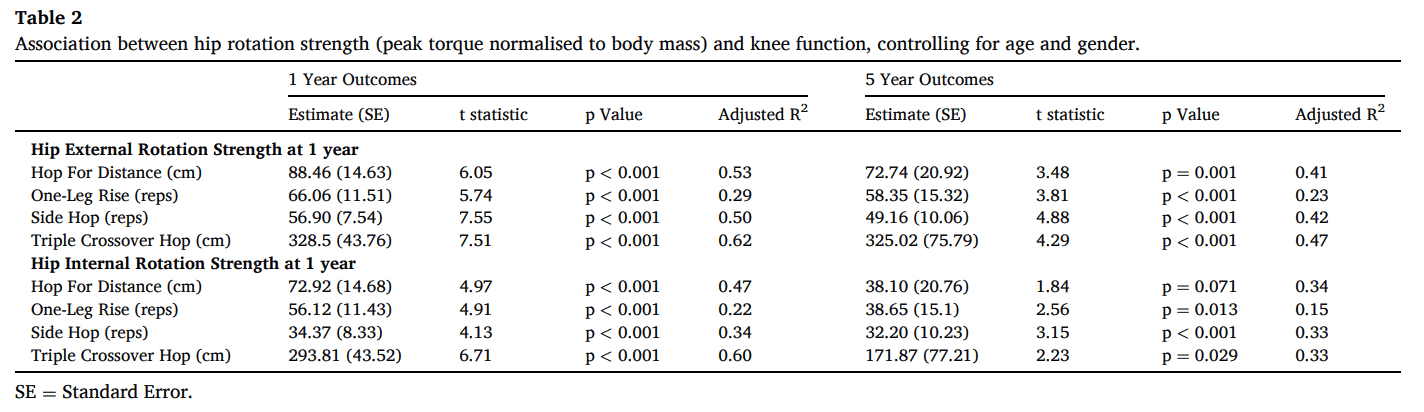
Lower external rotation hip strength after ACL reconstruction was associated with worse symptoms at 5 years, as measured by the KOOS and KOOS-PF scores. Lower internal rotation strength was only associated with worse symptoms measured with the KOOS-PF scores at 5 years.
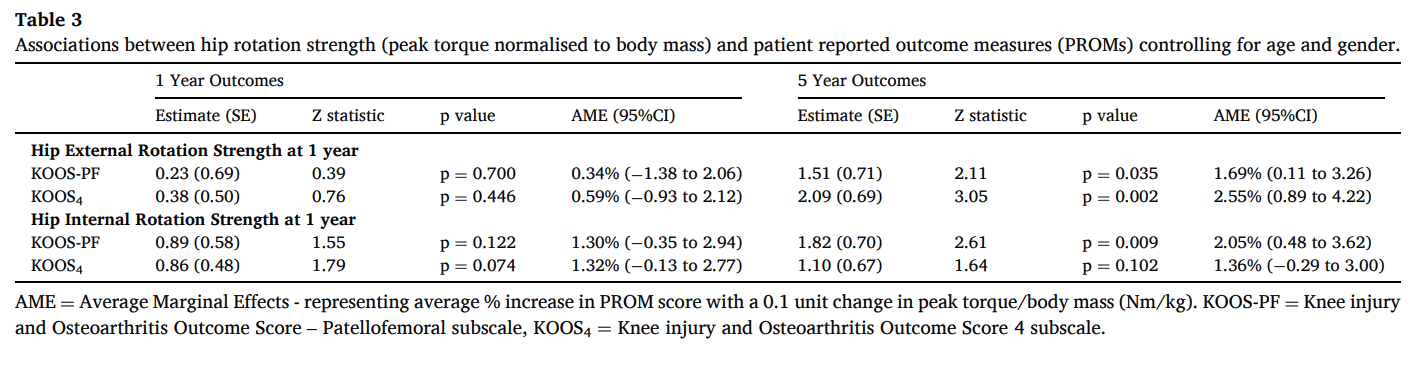
Better strength in internal and external rotation was associated with better performance on all functional tests at 1 and 5 years. The only exception was the absence of a relation between hip internal rotation strength and hop for distance at 5 years.
It seems that there was no association between hip internal or external rotation hip strength after ACL reconstruction and cartilage lesions in the patellofemoral or tibiofemoral compartments at 1 year. But the odds of worsening tibiofemoral cartilage were reduced with greater hip external rotation strength. Every 0.1 Nm/kg increase in hip external rotation strength was associated with a 0.61 times lower risk of worsening cartilage.
Questions and thoughts
Did the decreased strength come from inadequate rehabilitation or had the participants during the follow-up time decreased their level of sports participation? Did they bias strength training of their knee muscles but did they pay too little attention to more proximal muscles? All questions that emerge from this study.
Every 0.1 Nm/kg improvement in hip external rotation strength was related to a 0.61-fold decreased incidence of cartilage deterioration. However, this was not associated with radiographic osteoarthritis at 5 years. Yet, this may mean that the hip rotator muscles can exert important protective action against cartilage deterioration.
Talk nerdy to me
The data of the present study were obtained from a longitudinal cohort study that assessed functional, symptomatic, and structural outcomes after ACL reconstruction. As such, the current study did not calculate a sample size nor did it include a control group. Due to the observational nature of the study, we cannot conclude in which direction the effect lies. Nor can we say that lower strength was responsible for the worse KOOS scores since an association says nothing about a cause. Furthermore, the influence of other variables cannot be determined since the study did not control for confounders.
Take home messages
It appears that lower hip external rotation strength at one year following ACL reconstruction is associated with worse functional outcomes at the 5-year follow-up. However, the difference found was likely not clinically significant.
Reference
Additional reference
LEVEL UP YOUR DIFFERENTIAL DIAGNOSIS IN RUNNING RELATED HIP PAIN - FOR FREE!
Don’t run the risk of missing out on potential red flags or ending up treating runners based on a wrong diagnosis! This webinar will prevent you to commit the same mistakes many therapists fall victim to!



