High Intensity Resistance Training for Osteosarcopenic Elderly Men

Introduction
Osteosarcopenia is the simultaneous presence of osteopenia and sarcopenia. Exercise therapy might be effective in increasing bone mineral density (BMD) in women, as studies have shown. Few studies investigated men. This study aims to test if high-intensity dynamic resistance training (DRT) can be an effective means to increase BMD compared with a control group.
Methods
Individuals from a previous study were contacted. Those with the lowest skeletal muscle mass index (SMI) quartile. A total of 180 men were willing to participate.
The inclusion criteria were as follows:
- Community-dwelling men
- ≥ 72 yo
- Skeletal muscle mass index ≤ 7,26 determined by dual-energy X-ray absorptiometry (DXA) (= sarcopenia)
- BMD at the lumbar spine or total hip lower than -1 SD T-score (= osteopenia)
The exclusion criteria were:
- Secondary osteoporosis
- Hx of hip fracture
- (Osteo)anabolic and antiresorptive pharmaceutical therapy
- Glucocorticoid therapy > 7.5 mg/d during the previous 2 years
- Diseases that prevent dynamic resistance training
- Participation in resistance training
Forty-three men were eventually included and randomized into either the control or exercise group.
All participants were given vitamin D, protein, and calcium supplements. However, the exercise group received a higher dose of protein, 1.5–1.6 versus CG 1.2–1.3 g/kg body-mass/d, and were blinded for this. The dosage of calcium supplements followed national (German) guidelines.
The exercise group – obviously – received an exercise program. The program took about 45-50 minutes per session, twice a week, and included high intensity resistance training. The authors describe different phases:
Phase 1: four weeks of familiarization with the exercises followed by eight weeks of conditioning with a focus on education and adequate load selection.
Exercises included were: leg press, extension, curls, adduction, abduction, latissimus front pulleys, rowing, back extension, inverse fly, bench press, military press, lateral raises, butterfly with extended arms, crunches
Twelve exercises were applied per session. Eight thereof were performed for one set, four for two sets. Sets consisted of 8-15 reps of 5 seconds in total with proper intensity (not yet to failure). Ninety- to 120 seconds of rest were prescribed.
Phase 2: the single-set approach was started. Two blocks of four weeks with one week of rest at the end for both.
Four new exercises: calf raises, hip extension, pull-overs, and lateral crunches.
Fourteen exercises were applied per session with 90 seconds of rest between them. Participants were instructed to choose a load that ensured 5-10 reps with one rep in reserve (RIR) or 10-18 reps with two RIR. Movement velocity varied between sessions from very slow (9 seconds in total) to fast (4 seconds in total).
Phase 3: one third of the sets were conducted with an explosive movement in the concentric phase (not for back extensions). Adding to this, sets were performed until zero RIR. The explosive sets were terminated when explosiveness was no longer possible. This was used for sets ≤ 10 reps.
Phase 4: supersets were introduced for agonist and antagonist muscle groups. The sequence consisted of 2-3 sets with rest pauses of 30-45 seconds within.
Phase 5: drop sets were introduced with one decrease in load of 10-20% immediately after a maximal set or a set with one RIR. Drop sets referred to seven exercises included in the supersets. Rest pauses were 1 minute within and 2 minutes between supersets.
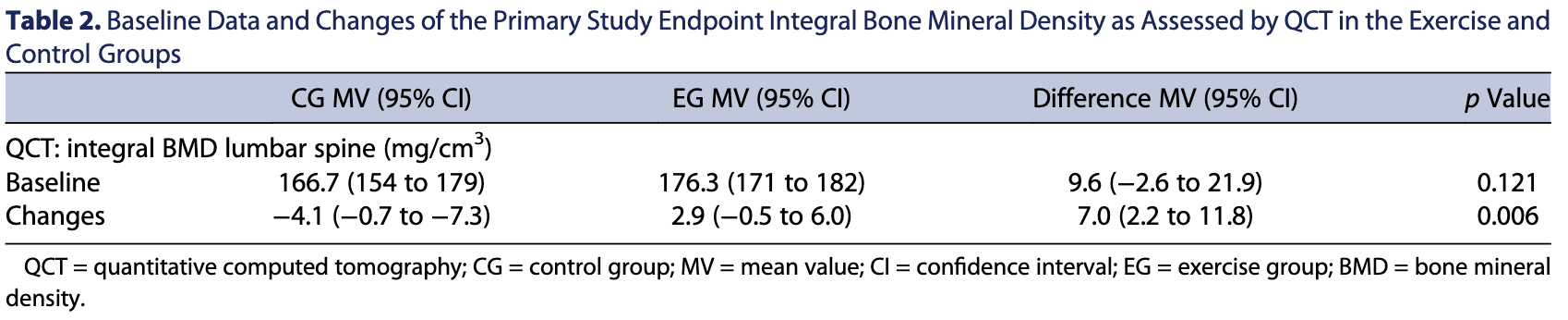
The primary outcome measure of the study was integral BMD at the lumbar spine after 54 weeks.
Results
Excellent compliance was achieved with an average of 102 sessions of 108. The average session time was around 45 minutes. Compliance with supplements was high as well. However, compliance for intensity (close to failure) was lower. The authors estimate that around one-fourth to one-third of sets were of inadequate intensity.
The primary outcome measure was the lumbar-spine bone-measure-density (LS-BMD) after one year. This measure decreased significantly in the control group and increased non-significantly in the exercise group. However, changes between groups were significantly.
Secondary outcome measures will not be discussed since the study had no statistical power for this.
Talk Nerdy To Me
Kudos to the authors, this is a great study. Statistical power was measured to find out how many participants were needed. Enough participants were recruited to measure LS-BMD after one year with 90% power. However, the authors did not correct the multiple comparison problem. This means that the measures for secondary outcomes and multiple time points should be interpreted with caution.
The study group consisted of men with a mean age of 78 years with normal to slightly overweight, according to their BMI. About half of the participants presented with three or more comorbidities and just one participant (5%) per group presented with diabetes mellitus type 2. The latter might be an underrepresentation of this population.
The program was highly structured, detailed, and progressive. The authors note in their discussion that this was a low-volume program. According to strength training principles in more younger folks this might be the case. The per-muscle volume could be concluded to be low as well. However, looking at the total muscle volume and the fact that we are looking at 78 year old men, one could say that this is not low volume.
A thing worth investigating might be what a cycle of impact training would do. Bones react to stress and activities with impact thus stimulating growth.
Now, we all know statistical significance does not equal clinical significance. The results suggest that strength training might mitigate osteoporotic effects seen in the control group. This is great, however, is it useful? Will it reduce fracture risks with falls? Will a longer-term program reduce fractures with falls? Will increased muscle mass and bone density due to such programs reduce injuries overall? How will the effects look in women since females suffer more greatly from osteoporosis? These are interesting questions.
Take Home Messages
- High-intensity strength training is feasible in an older male population
- It could be that strength training could counteract osteoporotic effects
Reference
MASSIVELY IMPROVE YOUR KNOWLEDGE ABOUT LOW BACK PAIN FOR FREE
5 absolutely crucial lessons you won’t learn at university that will improve your care for patients with low back pain immediately without paying a single cent