Does it Matter How You Explain Achilles Tendinopathy?

Introduction
Achilles tendinopathy is a condition characterized by an extended period of symptoms that may affect a person’s quality of life and ability to participate in sports or physical activity. Despite exercise-based rehabilitation being the go-to option, many people continue to have symptoms when discontinuing their rehabilitation. In this light, it is often thought to deliver exercise therapy combined with pain education so the individual learns about the condition. The biopsychosocial model is widely incorporated into rehab and research but often gets blamed for forgetting the “bio” part. In this study, the authors tried to compare pain education delivered through a biopsychosocial explanation versus pathoanatomical education which was more biomedically oriented, on the outcomes of pain and function.
Methods
This study sought whether it matters how you explain Achilles tendinopathy to a patient. Therefore, they compared participants with chronic Achilles tendinopathy who participated in an exercise program and were randomly allocated to receive either a biopsychosocial or a biomedical pain explanation on top. The primary aim was to compare the difference in pain and functional outcomes at 8 weeks.
Both people with midportion and insertional Achilles tendinopathy could be included when the Achilles tendon was the primary pain location. Symptoms had to be provoked by weight-bearing activities and rise to at least 3/10 when walking, doing heel raises, or hopping.
The participants were enrolled in an exercise program for 7 weeks where they received 6 to 7 supervised sessions of 30 minutes. The first session had a duration of 45 minutes. Those with aggravated pain during ankle dorsiflexion were given additional heel raises. During the second period between 9 and 12 weeks, the participants were instructed to perform home exercises.
The only difference between the groups was the content of the education program. The biopsychosocial explanation was based on selected content but emphasized a biopsychosocial perspective on the neurophysiology of pain. Further, it touched on the impact of pain catastrophizing and kinesiophobia. It promotes physical activity to improve pain to create lasting effects. Participants receiving the biomedical explanation of Achilles tendinopathy learned about the pathophysiology of the condition and biomedical sources of pain. Further, they had to apply the knowledge during participation in the tendon loading program. Similar to the other group, the program promoted participation in exercise as a means of improving overall physical health.
What did the exercise program consist of? For both groups, the same program was held. In phase 1, the emphasis of the program was on isometric exercises. Phases 2 and 3 focussed on heel raises and the spring function of the Achilles tendon, respectively. Progressions were made based on time and predetermined criteria based on symptoms and ability to complete the exercises, as depicted hereunder.
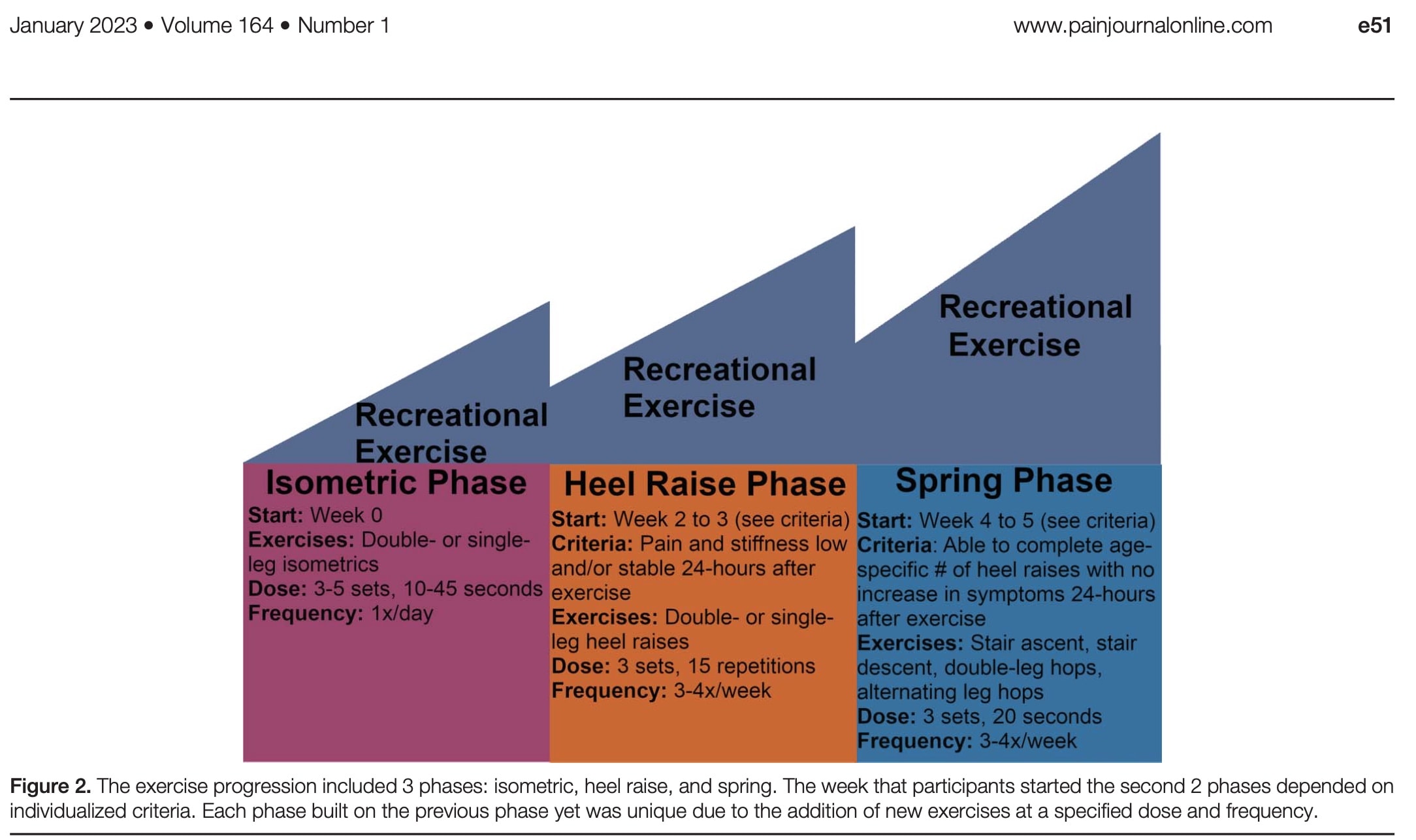
As both participants with midportion and insertional Achilles tendinopathy were included in the RCT, the heel raises were standardized to be performed on level ground without a decline phase. Participants were encouraged to participate in recreational exercise and to gradually increase this with the weeks going by. To promote this, modifications were given to minimize aggravation of their pain during participation in recreational activities. Examples of modifications were heel lifts, shorter stride lengths, and altering the duration of the activity.
The outcome measures were obtained at baseline and the primary endpoint of 8 weeks. A follow-up was held at 12 weeks. A total of 5 domains were assessed:
- Pain: movement-evoked pain during heel raises measured with the NPRS immediately following the movement. Here the minimally clinically important difference is 2 points.
- Self-reported function: Patient-Reported Outcomes Measurement Information System (PROMIS) tool. This tool has a minimally clinically important difference of 7.6-8.4 points.
- Psychosocial factors: measured with the Tampa Scale of Kinesiophobia (TSK-17). A score of more than 37 indicates elevated fear of movement and the minimally clinically important difference is 5.5 points.
- Performance-based function: Performance-based function tasks were completed in the following order: walking at a self-selected pace, walking at a quick standardized pace (Froude 471), heel raises, and hops. These movements were evaluated on good execution via 3D motion analysis.
- Central nervous system nociceptive processing: A sensory testing protocol using a pressure algometer was performed to determine the pressure pain threshold.
Results
Sixty-six participants with chronic Achilles tendinopathy were included in this RCT. They suffered from Achilles tendinopathy for on average 14 to 18 months in the biopsychosocial education and biomedical education groups, respectively. In both groups, slightly more people were affected by insertional Achilles tendinopathy. On average, they had sought care from 2 providers, most of whom were physiotherapists. They tried 5 treatments on average. More than 60% of them previously tried strengthening. It seems a pretty therapy-resistant population.
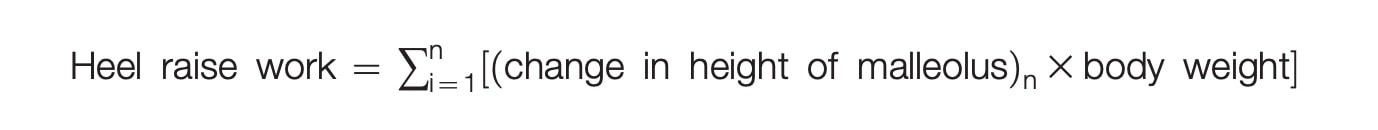
The groups were well balanced at baseline except for the heel raise work and hop height. Heel raise work was quantified as the sum of the change in ankle height times body weight for the maximum number of heel raises (n) that they were able to complete. In the group receiving biopsychosocial education, this was on average 619 Nm but in the group receiving the biomedically-oriented education, this equaled 834 Nm. Hop height at baseline was around 4 centimeters less in the group receiving biomedical education.
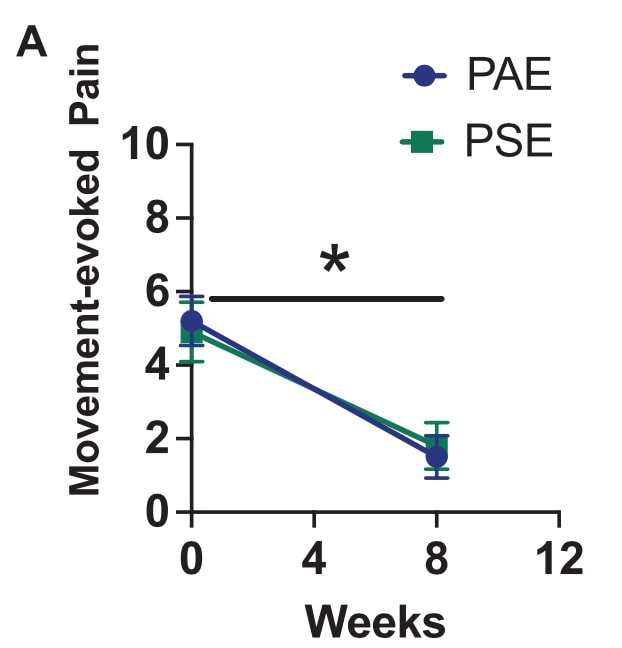
At eight weeks, biopsychosocial pain science education was not more effective than biomedical-oriented education. In both groups, similar improvements were seen in movement-evoked pain, without the superiority of one above another. On average, a 3-point reduction was observed from baseline to week 8.
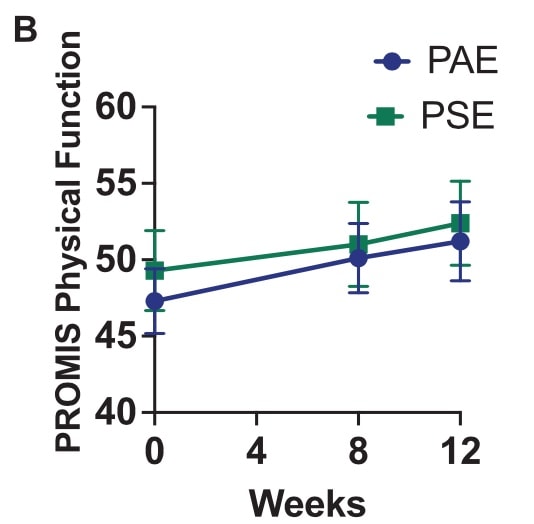
Function, measured with the PROMIS Physical Function, did not increase over time.
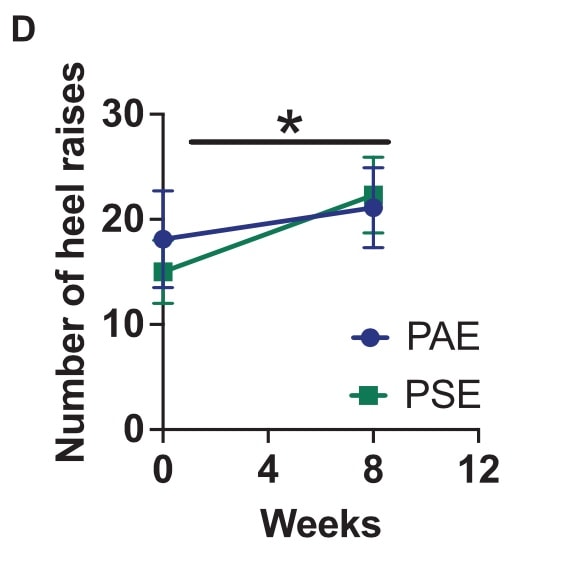
Both groups managed to improve their maximal number of heel raises over time, again without one group being superior to the other.
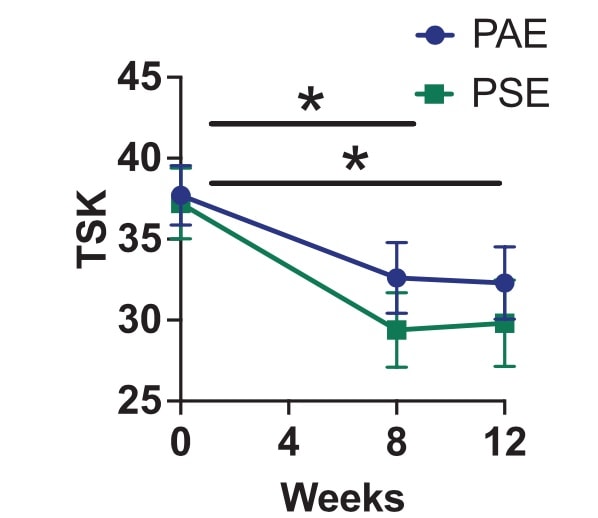
The reported level of kinesiophobia decreased throughout the study in both groups and this improvement was maintained at 12 weeks. No improvements were seen in the conditioned pain modulation measured with the PPT.
Questions and thoughts
- What was done when the pain flared up? Exercises from the phase the patient was in were reduced or replaced with exercises from the previous phase. For example, if a participant’s symptoms increased during the heel raise phase, then the participant was instructed to reduce the height of the heel raise motion, decrease the number of repetitions, and/or replace the heel raises with isometrics until symptom aggravation resolved.
- The PROMIS Physical Function did not improve significantly while VISA-A did. There was no difference between participants who had insertional versus those with midportion Achilles tendinopathy. While both tools assess physical function, there are some differences between them. The PROMIS Physical Function tool is a more general measure that can be used in various health conditions and populations, whereas the VISA-A questionnaire is specific to Achilles tendinopathy.
- The PROMIS tool utilizes computer adaptive testing, which allows for efficient and precise assessment of physical function, while the VISA-A questionnaire consists of a set of fixed items.
- The authors stated that this was potentially due to a ceiling effect in the PROMIS tool.
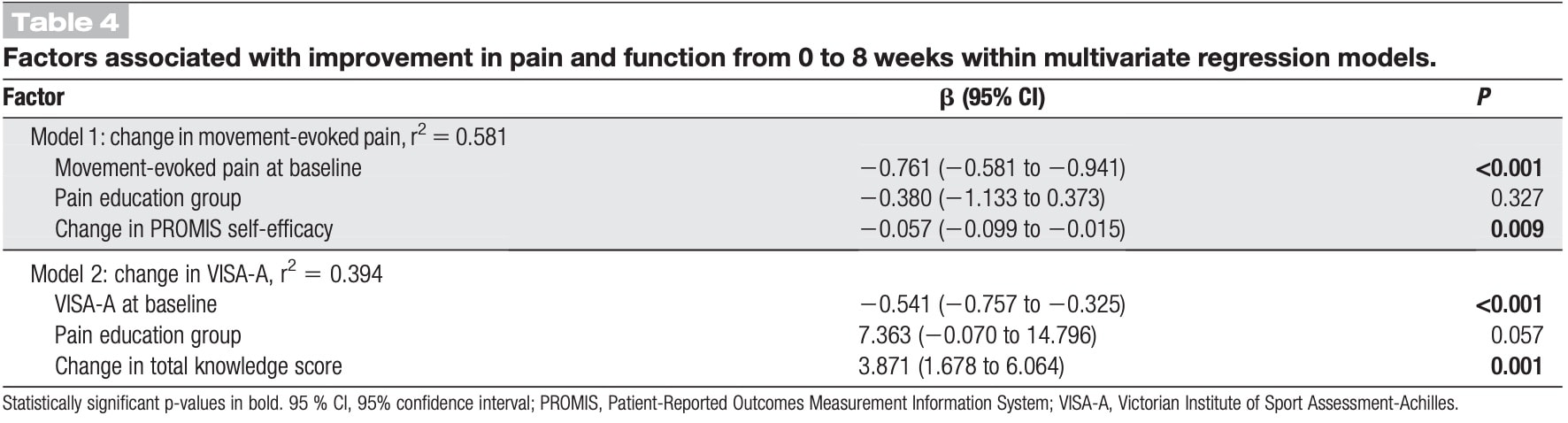
- What factors determined improvement in this population? A multivariate linear regression analysis was done and revealed that a higher baseline movement-evoked pain and a greater increase in PROMIS self-efficacy were associated with a greater reduction in movement-evoked pain. For every 10-point increase in self-efficacy, there was a 0.6-point reduction in movement-evoked pain. This model explained nearly 60% of the variance in the improvement of movement-evoked pain. Model 2, as depicted hereunder looked at the change in VISA-A, but as this was not a primary outcome, I’d say it is not opportune to consider this.
- Maybe not everyone needs pain science education. It is not about a one-treatment-fits-all approach. Although I am the first to explain things to my patients when they ask for an explanation, I certainly do not educate them about the neurophysiology of pain every time. Sometimes you’ll give more attention to the bio-part of the explanation. In other cases, the psycho or social aspects are more important. Pragmatic studies could shed an important light on this.
- In a recent systematic review and meta-analysis, Siddall et al., 2022 found greater reductions in pain and disability when pain education was combined with exercise. Why does this study show other results? When reading the paper by Siddall, you can see that they included a different population than those having Achilles tendinopathy. They talk about “chronic musculoskeletal pain”, but when you delve into the study, you see that they only included populations having neck, back, and spinal pain.
- What can we do as physiotherapy professionals when we know our patient already sought advice and treatment from another physiotherapist? I’d generally say: try to examine what the earlier rehabilitation looked like, in terms of what was done, for how long, and how. Gather as much information to try to find the “missing link” in that earlier rehabilitation. Often I hear, that they completed 18 sessions of physiotherapy in 6 weeks. Since the condition of Achilles tendinopathy is known not to resolve quickly, spreading these sessions over months and teaching your patient to self-manage in between sessions seems much more valuable. Physiotherapy is stepping away from treating patients, toward guiding and empowering patients.
- Biomedical education was considered a placebo treatment. I doubt this is a real placebo as the patient gets to know more about the condition and receives an explanation of what may be causing pain. The scope is different from the biopsychosocial point of view but carries important information about the pathology itself.
Talk nerdy to me
- Is it possible that a carry-over effect occurred? The paper did not provide information that a potential carry-over effect between groups had or had not occurred. What they did check upon was blinding, which was good as more than 50% of the participants in both groups believed that they received the education program that the study team thought was most effective.
- To create consistency in the program, the heel raise exercises were not performed in decline but were performed on level ground. This was done to avoid pain and irritation in people having insertional Achilles tendinopathy. A subdivision between insertional and midportion Achilles tendinopathy may have been better suited.
Take home messages
This study investigated the effect of pain education delivered through a biopsychosocial explanation versus pathoanatomical education on the outcomes of pain and function. The pain education was integrated into an exercise program. From the outcomes, it appears that it does not matter how you explain Achilles Tendinopathy to your patient. At eight weeks, neither biomedical-focused education nor education in biopsychosocial pain science was more beneficial. Similar reductions in movement-evoked pain were observed in both groups, without any clear favoring of one group over the other. Between baseline and week 8, an average 3-point decline was seen.
Reference
Additional reference
WHAT TO LOOK FOR TO PREVENT HAMSTRING, CALF & QUADRICEPS INJURIES
Whether you’re working with high-level or amateur athletes you don’t want to miss these risk factors which could expose them to higher risk of injury. This webinar will enable you to spot those risk factors to work on them during rehab!



