Effectiveness of Pain Education and Exercise for Carpal Tunnel Syndrome Delivered Through Telerehabilitation

Introduction
Pain education is everywhere, and that is a good thing. It has been shown to reduce levels of anxiety and distress in various musculoskeletal conditions. When you inform (or educate, what is in a name) your patient well, you already have an advantage despite the type of treatment you opt for. More and more evidence points to the relevance of self-management. As such, physiotherapy is turning away from “treating” patients and moving on to guide someone through a certain pathology. In this aspect, I chose to review this RCT as it combined both. The application of pain education and exercise for carpal tunnel syndrome delivered through telerehabilitation.
Methods
In this RCT, pain education and exercise for carpal tunnel syndrome were compared against exercise only. Both interventions were delivered through telerehabilitation.
Participants were between the ages of 18 and 60 years and had moderate to severe carpal tunnel syndrome. This definition was established according to the clinical practice guidelines of the Academy of Orthopaedic Physical Therapy and the Academy of Hand and Upper Extremities Physical Therapy. We covered this practice guideline on our YouTube channel, which you can watch here. Further, their symptoms were present for at least 3 months and could have been unilateral or bilateral in presence.
The included participants were randomized on a 1:1 allocation ratio to receive exercise only compared to pain education and exercise for carpal tunnel syndrome. Both groups received the exercise therapy program through telerehabilitation. Three telerehabilitation sessions were supervised by physiotherapists every 15 days.
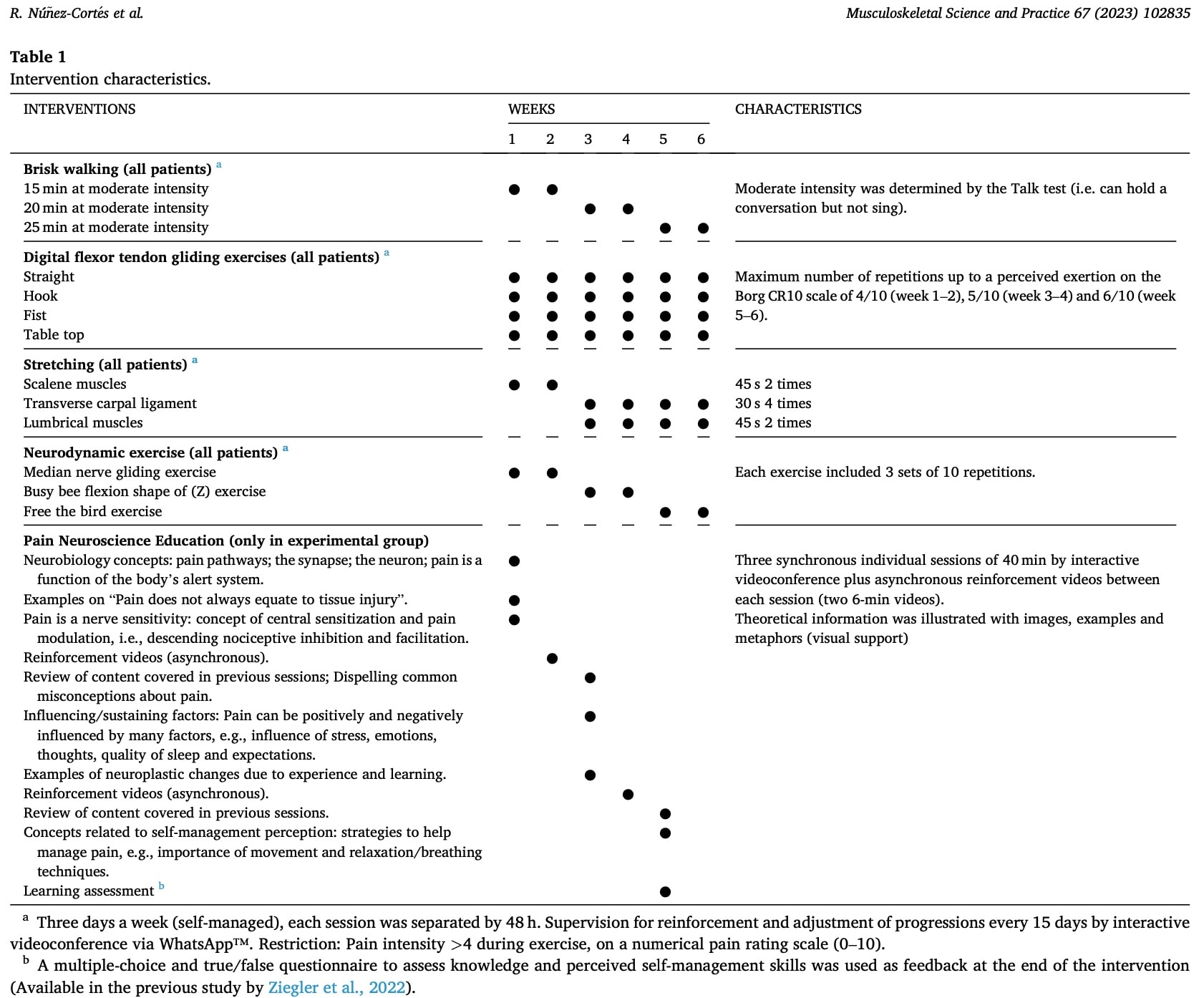
In the exercise group participants performed aerobic exercise, digital flexor tendon gliding, neurodynamic home exercises, and self-stretching.

These exercises were performed three times per week for 6 weeks, with a 48-hour interval between each session. Each exercise session lasted approximately 30 min. In total, 15 self-managed and 3 supervised sessions were held.
In the group receiving pain education and exercise for carpal tunnel syndrome, participants received 3 additional sessions of pain neuroscience education. The table hereunder depicts the detailed program for both groups.
Pain intensity was the primary outcome of interest and this was measured using the NPRS at 6 weeks and 12 weeks. Other outcome measures included the Pain Catastrophizing Scale (PCS), Tampa Scale for Kinesiophobia-11, Boston Carpal Tunnel Questionnaire (BCTQ), Hospital Anxiety and Depression Scale (HADS), EuroQol5-dimensions (EQ-5D), and the Patient Global Impression of Change Scale (PGICS).
Results
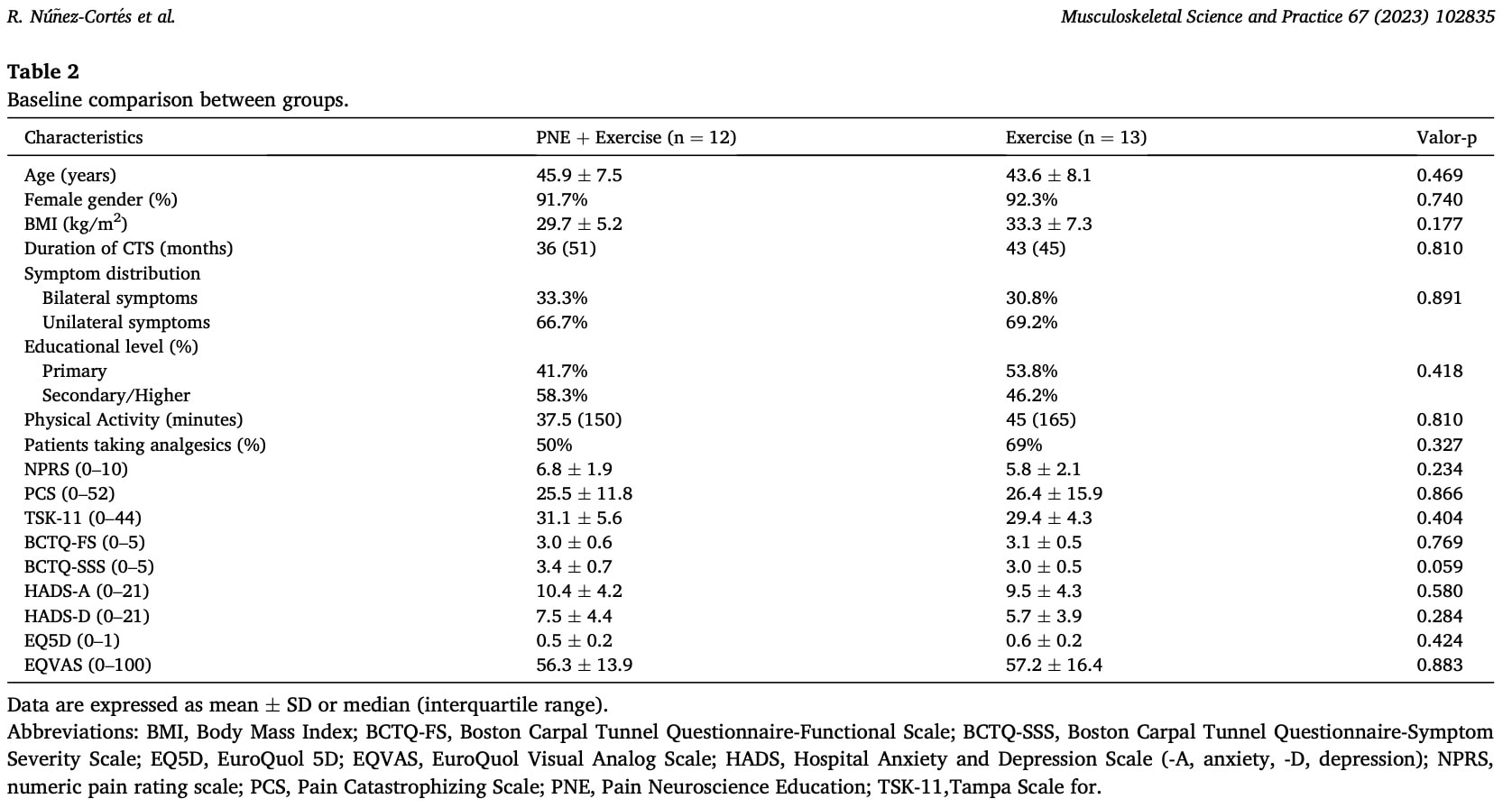
The analysis of the baseline characteristics revealed no significant differences between the groups at the start of the study.
The study wanted to know whether pain education combined with exercise was better than exercise alone. So they tried to rate the between-group effects.
The paper stated that there was no interaction effect or main effect for group, but a main effect for time was observed. Further, they state: “Significant and clinically relevant differences in NPRS were observed at week 6 in the PNE + exercise group (MD: 2.0 points, 95% CI: -3.8 to −0.2). The exercise group showed no improvement at any time point”.
Questions and thoughts
- This study included participants who were awaiting surgery and had complaints for a long time. No differences were observed between the pain education plus exercise and exercise-only group for the primary outcome. Yet, patients receiving the combined intervention were more satisfied than the exercise group at 6 weeks. This effect disappeared at 12 weeks. This may have been the result of more attention, and care received, response bias… rather than a true difference. Further, this outcome was not the primary outcome, and the study was not powered to detect such a difference.
- The current study used many patient-reported outcome measures. I even wonder how they managed to get them all filled by the participants. In practice, I would certainly not use so many in a patient of mine. Rather I’d focus on one or two outcomes they’d find relevant.
- The secondary outcomes revealed significant interaction effects for kinesiophobia. Looking at the data reveals that at weeks 6 and 12, the mean between-group difference was −5.2 points [95% CI: 9.7 to −0.6; p = 0.028] and −5.7 points [95% CI: 10.8 to −0.5; p = 0.034], respectively. This may indicate that pain education combined with exercise for carpal tunnel syndrome is effective in reducing fear of movement in this population, but as it is a secondary outcome, caution in the interpretation of this finding is warranted.
- Considering the severity of symptoms, a significant interaction effect found a difference between the groups, but this was not clinically meaningful. As this is a secondary variable for which the trial was not powered, this difference may have occurred by chance.
Talk nerdy to me
- No baseline differences were observed between the groups, meaning the authors managed to create a homogeneous sample
- The primary analysis failed to find a between-group difference for the primary outcome of pain intensity. Yet, the study highlighted the benefits of including PNE in telerehabilitation interventions for patients with CTS. This is contradictory and misleading.
- The trial resulted in a significant within-group improvement at 6 weeks that was clinically relevant in the group receiving pain education and exercise for carpal tunnel syndrome.
- However, the purpose of this study was to evaluate the benefits of adding pain education to exercise by comparing it to exercise alone.
- Since there were no differences between groups, I think the article is misleading by emphasizing the importance of pain education combined with exercise. The way they formulate it seems as if the group receiving the combination of education and exercise was better improved at 6 weeks compared to the exercise group. Instead, this is a within-group difference, but that is not what this study ought to be about. This is misleading and not correct. This is clearly explained by the study by Altman et al., in 2011.
Take home messages
Pain education and exercise for carpal tunnel syndrome were not more effective than exercise alone for reducing pain intensity. Although mentioned and highlighted, this reflects the interpretation of a within-group improvement where the study wanted to compare between-group effects. The study indicated that adherence to the program was high and that participants were satisfied with the way of receiving telerehabilitation. Combining pain education and exercise may be useful for reducing kinesiophobia, but this was a secondary outcome and should be further tested.
Reference
Additional reference
HOW NUTRITION CAN BE A CRUCIAL FACTOR FOR CENTRAL SENSITISATION - VIDEO LECTURE
Watch this FREE video lecture on Nutrition & Central Sensitisation by Europe’s #1 chronic pain researcher Jo Nijs. Which food patients should avoid will probably surprise you!



