How do knee cartilage lesions evolve over 4-6 years?

Introduction
Meniscal injuries get frequently operated and here arthroscopic repair or resection are the main two options. We know from other research that saving the meniscus has a beneficial impact on the prevention of osteoarthritis. Sometimes cartilage lesions are present in those who undergo arthroscopic surgery for their meniscus lesion. This study was curious about the evolution of cartilage lesions and patient outcomes in those who had meniscus surgery.
Methods
To examine the evolution of cartilage lesions and patient outcomes the prospective Knee Arthroscopy Cohort Southern Denmark (KACS) cohort was used to answer the research question. In this study, 641 participants (mean age 49 years (range 18-77; 43% women) were followed from the moment they underwent arthroscopic meniscal resection or repair.
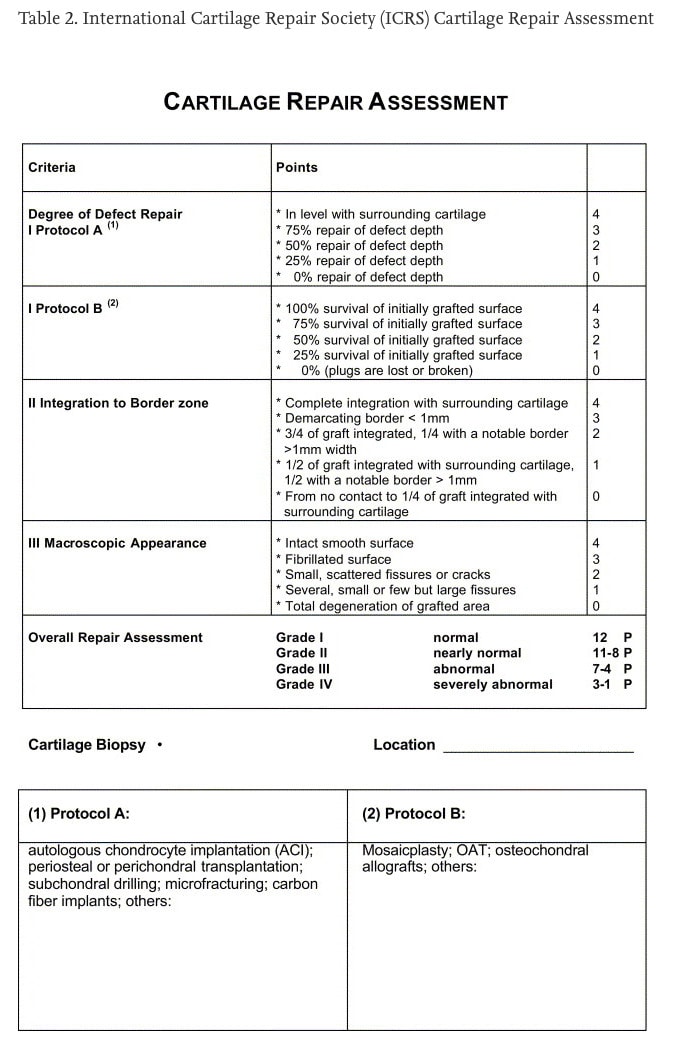
During the surgery, the presence of cartilage lesions was rated by the surgeon using the International Cartilage Repair Society (ICRS) scoring system. This scoring system ranges from 0-4 with higher scores representing more cartilage damage. The cartilage lesions were located in the medial tibiofemoral, lateral tibiofemoral, and patellofemoral compartments of the knee. Four categories of cartilage lesions were defined:
- no cartilage lesions (ICRS < Gr. 2 throughout the knee);
- isolated patellofemoral cartilage lesions (ICRS ≥ Gr. 2 in the patellofemoral compartment only);
- isolated tibiofemoral cartilage lesions (ICRS ≥ Gr. 2 in the tibiofemoral compartments only);
- combined cartilage lesions (ICRS ≥ Gr. 2 in both the patellofemoral and tibiofemoral compartments)
Pre-operatively, at 3 months and 12 months, the Knee injury and Osteoarthritis Outcome Score (KOOS) was completed by the participants and this was repeated at 4 to 6 years post-operatively. The KOOS includes 42 questions and has 5 subscales: Pain, Symptoms, Activities of Daily Living (ADL), Function in Sport and Recreation (Sport/Rec), and Quality of Life (QoL). An aggregate score was computed consisting of all information from the subscales except from the ADL subscale. Higher KOOS scores indicate better outcomes.
Results
The evolution of cartilage lesions and patient outcomes was followed in 630 participants. Nearly half of them were female (44%), their mean age was 49 (SD: 13) years, and their BMI was 27.3 (SD: 4.4) kg/m2. Five hundred ninety participants had meniscal resection and 33 had their meniscus repaired. Seven participants (<1%) had both a resection and repair of the meniscus.
Cartilage lesions could be defined in half of the sample during surgery (55%). The most common pattern was combined patellofemoral and tibiofemoral cartilage lesions (n = 207, 33%), followed by isolated tibiofemoral (n = 119, 19%) and isolated patellofemoral (n = 23, 4%). At this moment, the KOOS scores were similar across all groups. People with cartilage lesions had slightly lower baseline KOOS scores, but this difference was only statistically significant in the group with the combined patellofemoral and tibiofemoral cartilage lesions at this point.
Changes over the study period were similar across groups and here also, the group without cartilage defects had higher scores at all time points. The participants with no cartilage lesions improved the most, on average with 27.4 points (95%CI: 25.0, 29.8) and that was a mean improvement of 57%. The same extent of improvement from baseline was seen in the combined patellofemoral and tibiofemoral group (57%), but here the within-group change was somewhat lower, with 24.4 points (21.7, 27.2). The participants in the isolated patellofemoral cartilage lesion group improved by 21.2 (13.0, 29.5) points which was a 48% improvement from baseline. The isolated tibiofemoral group improved by 22.4 points (18.7, 26.1) over the 4-6 years, which was a 49% improvement from baseline. At the final follow-up, all three groups with cartilage lesions had statistically significantly lower adjusted mean KOOS scores compared to the no-lesion group, with worse mean KOOS ranging from -6.8 (-11.4, -2.2) in the isolated tibiofemoral group, to -7.6 (-11.7, -3.6) in the combined lesions and -9.8 (-18.5, -1.1) points lower in the isolated patellofemoral group. This difference compared to the no lesion group is however not clinically relevant as the minimally clinically important difference of the KOOS is reported to be at least 8 to 10 points.
Questions and thoughts
An interesting finding is that 94% of the participants had a meniscus resection, and only 5% had meniscal repair! This is surprising because the preferred option is to save the meniscus as much as possible. Of note is that these results can therefore only be generalized to participants with meniscal resection. Secondly, this study followed patients who had a meniscal injury and who had no previous or planned surgeries for the anterior or posterior cruciate ligaments.
Secondary outcomes included the individual subscales of the KOOS and the Patient Acceptable Symptom State (PASS). The individual subscales of the KOOS improved in all participants.

The PASS determines the satisfaction of the patient with their current knee function. In case the patient was not satisfied with the outcome, they were asked whether they considered their treatment to have failed. Of the 630 participants, 149 were unsatisfied with the outcome after surgery. This is nearly 1 in 4 people reporting an unsuccessful outcome after meniscus resection (and to a very small extent after meniscus repair). The probability of having a satisfactory outcome (as determined by the PASS) was highest in the group without cartilage lesions. Here the probability of satisfaction was 75%, compared to 60% in the isolated patellofemoral joint cartilage lesion, 64% in the isolated tibiofemoral joint cartilage lesion, and 65% in the combined joint cartilage lesion groups. These lower percentages of successful outcomes were not statistically significant, but give an idea of how pain, symptoms, ADL, participation, and quality of life in people with different cartilage lesions may progress over time. The authors report that among those reporting to be unsatisfied with the outcomes after 4-6 years, the estimates of the percentages considering their treatment to have failed were very imprecise. This impeded a detailed interpretation according to the authors as they concluded the confidence intervals were wide and thus imprecise. Generally, when looking at the table from the supplementary data, those with cartilage lesions to the tibiofemoral joint with or without cartilage lesions at the patellofemoral joints (combined) reported a higher probability of treatment failure. Surprisingly, the lowest probability of reporting the treatment to have failed wasn’t seen in the group without cartilage lesions, but in the group with isolated patellofemoral lesions. This may be possibly due to the imprecise interpretation of the results, as the authors mentioned. But it could also have been possible that the group of people who were informed about a cartilage lesion present in the knee had undergone more engagement in activities to keep the knee joint cartilage healthy. Maybe they were told to remain active, to lose weight, to engage in mobility and strengthening exercises or activities and hence had a better influence on their cartilage health. On the other hand, those people who had been told to have no cartilage lesions may have engaged less in these lifestyle changes. This is however not examined in the current study but may be a possible explanation for the differences in successful outcomes or treatment failure. Those with a patellofemoral cartilage injury and a concurrent meniscus resection may have had a better prognosis since they did not have a tibiofemoral cartilage injury. Perhaps they had this surgery on their meniscus injury since this injury led to pain and decreased function, and perhaps they had a better functioning knee again after this meniscus resection compared to the group with a tibiofemoral cartilage injury, who could have experienced residual symptoms after this surgery. The sample size of the isolated patellofemoral lesion group was very small (23 participants) and this may also have influenced the findings. Important to note is that the combined lesion group had statistically significantly lower KOOS scores at baseline, compared with the other groups.

Unfortunately, we do know nothing about these participants over the course of the 4-6 year follow-up. What had they done during these years? Did they engage in adopting a more healthy or active lifestyle? Did they have postoperative rehabilitation? Maybe some did, some did not, and these are all possible confounding factors that should be examined in other research.
Talk nerdy to me
This study examined the evolution of cartilage lesions and patient outcomes in individuals undergoing meniscus surgery. At baseline (during the surgery), the extent of the cartilage injury was reported according to the International Cartilage Repair Society (ICRS) scoring system. This is however a scale developed to rate the quality of the cartilage repair. However, these scores were further dichotomized to whether there was or was no cartilage injury present during the surgery (which was the baseline measurement). It would have been interesting to see how the cartilage had evolved over time and whether this was related to the patient outcomes but hasn’t been reviewed here. Of course, they couldn’t use the same procedure to classify the extent of the cartilage lesions (surgery), but the use of MRI may have been interesting. The reliability of the scoring system used was reported to be good with an ICC of 0.83, thus they used an accurate measurement tool to classify cartilage lesions.
Sensitivity analyses did not change the conclusions. In these analyses, they looked at whether participants aged 40 or more had other outcomes than those younger. Or if there were differences between the people undergoing resection versus those undergoing meniscus repair.
Interestingly, during the study period, 26% of participants were lost to follow-up. This is a large proportion of the sample and can be questioned, as the only requirement for participation in the follow-up measurements was to fill in the patient-reported questionnaires. How can it be explained that such a large number of people decided not to participate anymore when only little effort was required from them? Were they unsatisfied with the outcomes to a greater extent than those who remained in the study? This remains unclear, unfortunately. Another thing remaining unclear to me is why the KOOS ADL subscale was restrained from the aggregate KOOS score.
Take home messages
Important to take away from this research is that in all participants over the course of the 4-6 year follow-up, improvements were seen on all KOOS subscales. Even those with cartilage injury documented during surgery may expect improvements in pain and knee symptoms, participation in sport and recreational activities, and in their daily life functioning and quality of life. The message to these patients with cartilage defects should not be very pessimistic. Yes, they may have slightly lower scores compared to people without cartilage injuries, but these differences were not significant. Thus the evolution of cartilage lesions and patient outcomes after meniscus surgery in those with documented cartilage lesions during surgery is favorable.
Reference
Additional References
THE ROLE OF THE VMO & QUADS IN PFP
Watch this FREE 2-PART VIDEO LECTURE by knee pain expert Claire Robertson who dissects the literature on the topic and how it impacts clinical practice.



