Cervicovestibular exercises in Adults with Mild Traumatic Brain Injury

Introduction
A concussion or mild traumatic brain injury can lead to prolonged symptoms of somatic, cognitive, and emotional origin. These symptoms can negatively impact daily functioning and participation in sports. The symptoms are thought to result from injury to the central nervous system, but they can be complicated by cervical spine and/or vestibular problems. One of the primary therapies, as confirmed by a clinical practice guideline by Quatman-Yates et al. and the systematic review by Langevin et al. in 2020, is a symptom-guided aerobic exercise (SLAE) program.
“Aerobic exercise training has been associated with faster symptom resolution and rate of return to sport, as well as improved neurologic recovery when used alone or in conjunction with other impairment-specific active rehabilitation therapies.” – Quatman-Yates et al. (2020)
Symptom-guided aerobic training is directed by symptoms, whereby aggravation of symptoms beyond a modest level should result in exercise session termination, while the absence of symptom aggravation can give justification for increasing exercise intensity and duration. It has previously been demonstrated to be effective among the suggested therapies following a concussion. However as some smaller RCTs have shown that cervicovestibular rehabilitation could decrease the time to return to sport, the current study’s authors wanted to examine its added value when combined with symptom-guided aerobic training.
Methods
Adults who sustained a concussion were recruited. The concussion diagnosis was based on the consensus statement on concussions in sports from the 5th international conference in Berlin.
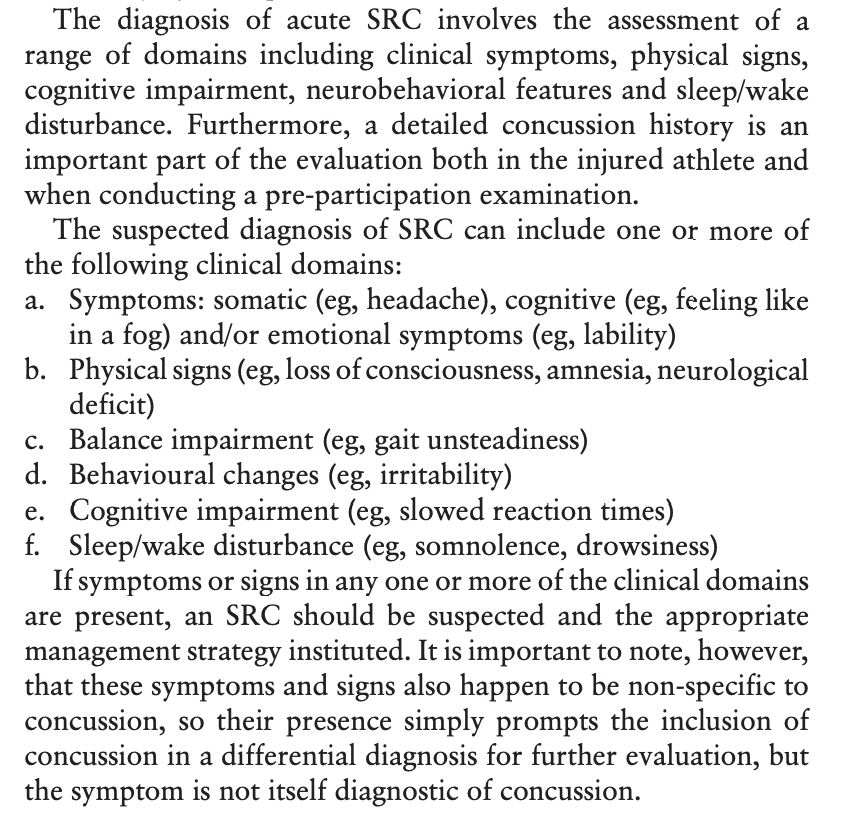
Participants could be included if they sustained a mild traumatic brain injury from a concussion in the past three to twelve weeks and experienced symptoms of dizziness, neck pain, and/or headaches that started 72 hours or less after the trauma. They had to present with at least one abnormality during the cervical physical examination (e.g., tenderness or spasm, or pain on segmental testing, or reduced motion), vestibular evaluation (e.g., Dix Hallpike or vestibulo-ocular reflex [VOR] tests), or ocular motor evaluation (e.g., convergence, smooth pursuits, or saccades).
Further, they had to have at least one of the following cognitive symptoms that started 72 hours or less after the trauma:
- feeling slowed down,
- feeling like in a fog,
- ‘‘don’t feel right,’’
- difficulty concentrating,
- difficulty remembering,
- confusion
During six weeks, the participants received eight supervised treatment sessions from a team of physiotherapists, kinesiologists, and neuropsychologists. These sessions comprised symptom-guided aerobic exercise in the control group. The experimental group performed the same symptom-guided aerobic exercise but with the addition of cervicovestibular exercises. Both groups got the recommendation to continue their exercises after the 6 weeks of supervised training.
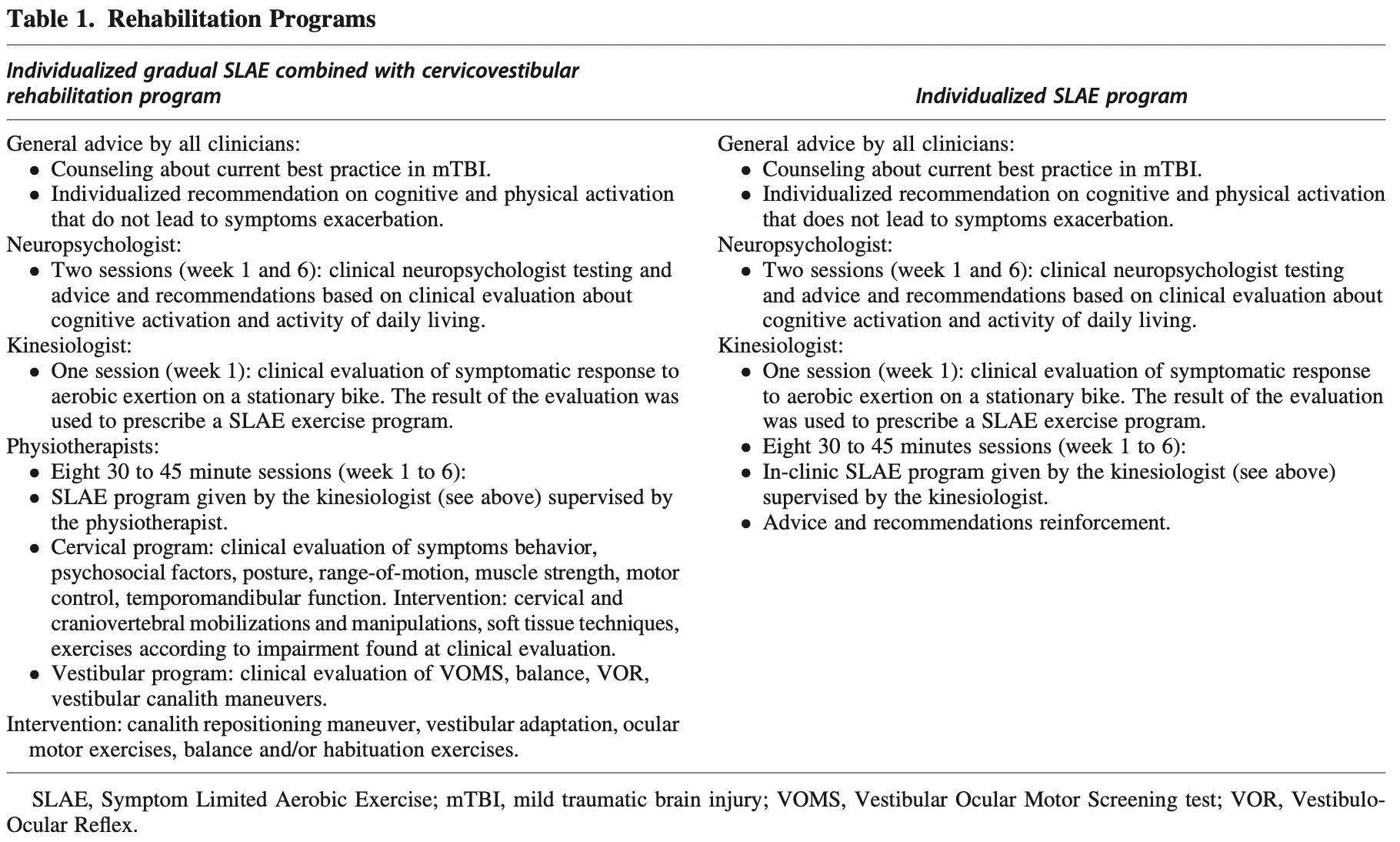
The exact components of the rehabilitation were at the discretion of the treating therapist and based on the results of the initial assessment. In the control group, the sessions were guided by the kinesiologist, while in the experimental group, the sessions were led by two physiotherapists.
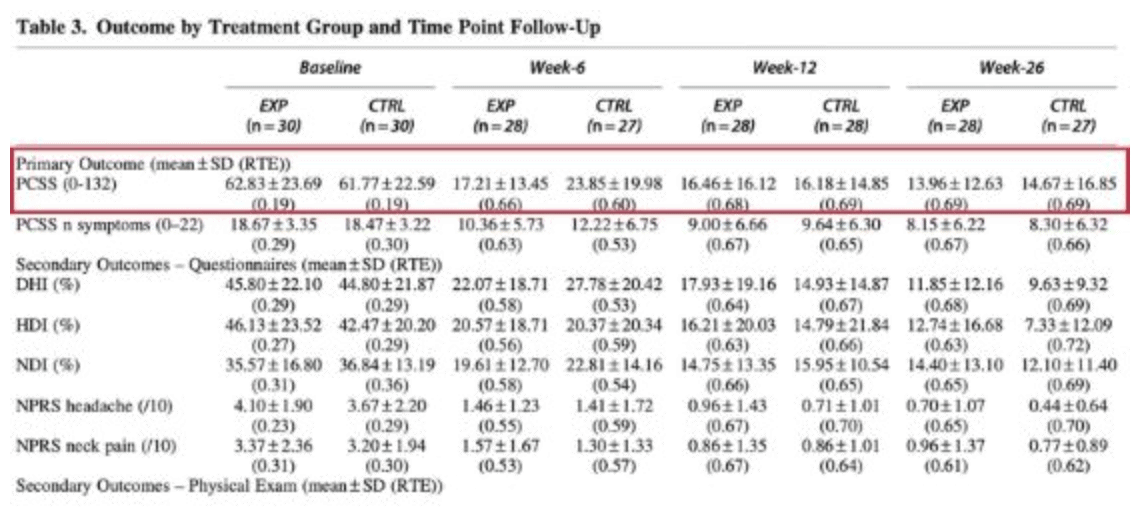
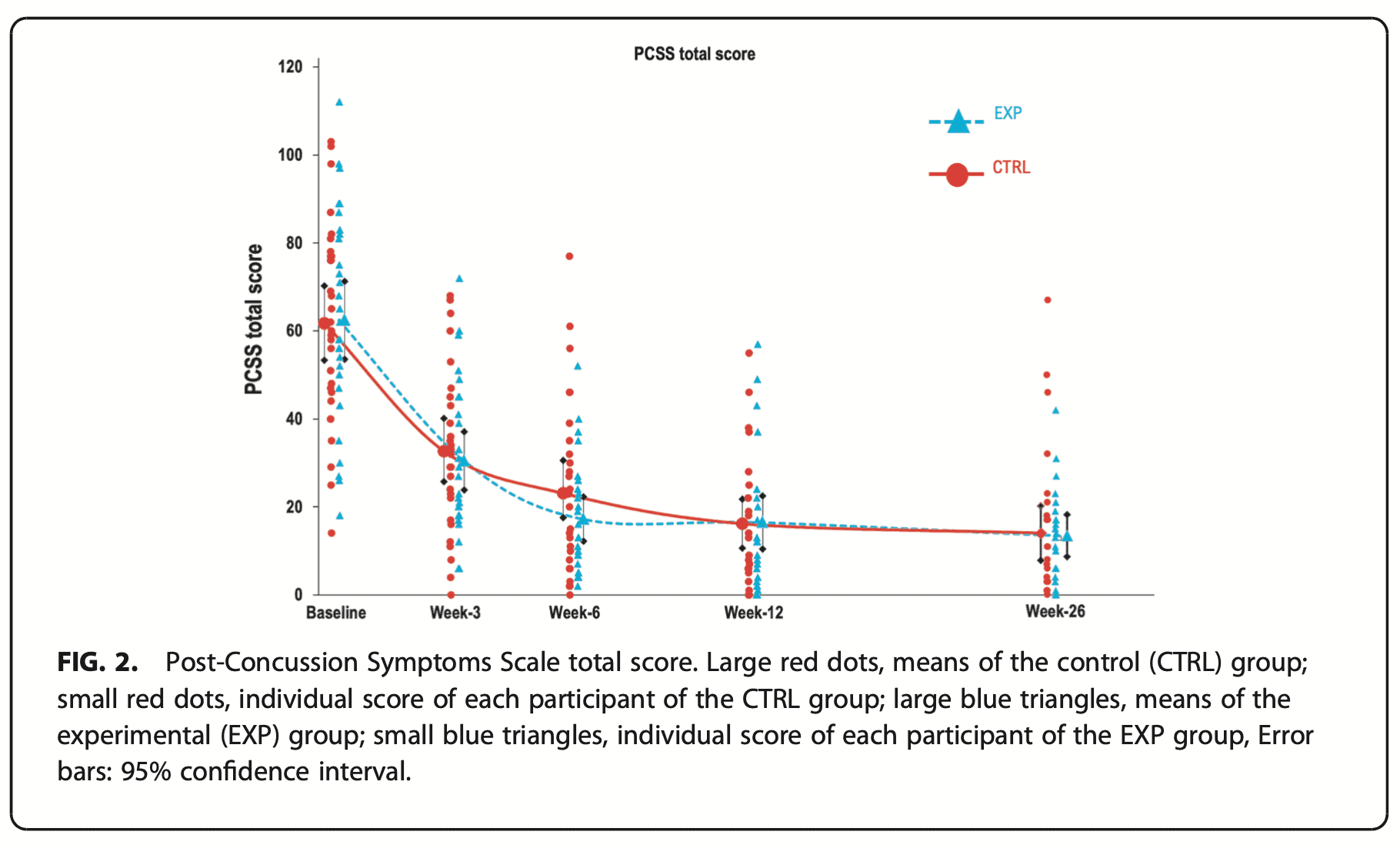
The primary outcome was the Post-Concussion Symptoms Scale (PCSS). It is a reliable and valid tool for evaluating self-reported symptoms in athletes with known or suspected concussions. The PCSS generates a severity score out of a total of 132 points and has been used to stratify concussion patients into symptomatic and asymptomatic groups. Higher scores represent more severe symptoms. This questionnaire was filled at 3, 6, 12, and 26 weeks.
Results
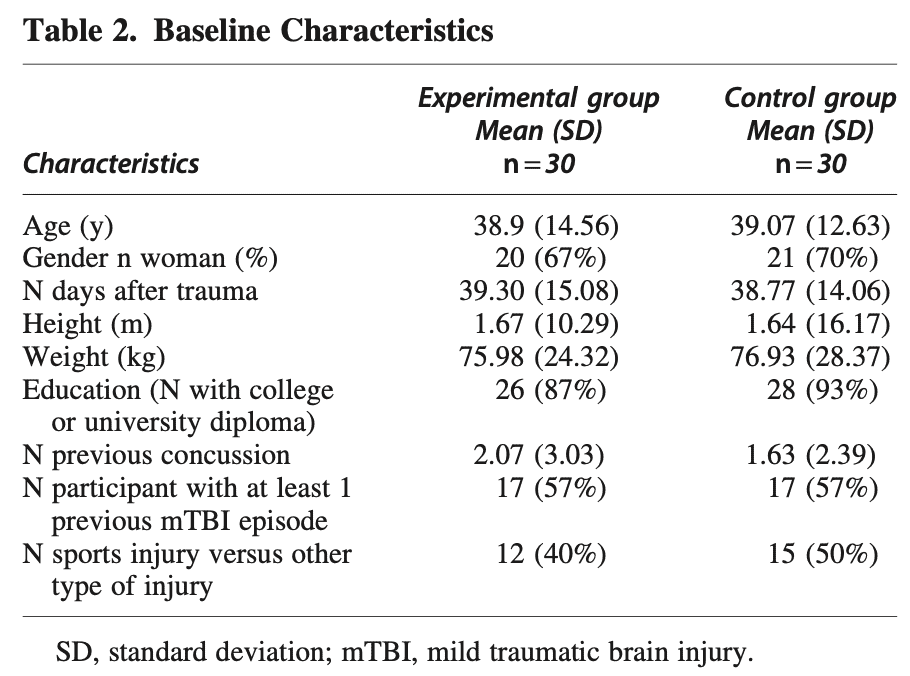
A total of sixty participants were included in the trial and equally divided into either the control or intervention group. They were similar at baseline.
The results indicated that both groups improved from baseline to weeks 6, 12, and 26. There were no significant between-group differences. The improvement in the PCSS is displayed in the table hereunder. The improvements largely exceeded the minimal detectable change (MDC) of 12.3 points of the PCSS.
Questions and thoughts
Based on the results, the PCSS total score improved in both groups at weeks 6, 12, and 26. There was no significant between-group difference. It means the control group performing symptom-guided aerobic exercise and the intervention group, who also participated in the aerobic program plus cervicovestibular exercises, improved. Therefore, it appears that the addition of cervicovestibular exercises should not be the main focus. Participating in an aerobic exercise program guided by the patient’s symptoms is the go-to treatment.
Because both groups achieved large improvements beyond the minimal detectable change of 12 points on the PCSS, the aerobic exercise program was likely able to improve the symptoms beyond a clinically relevant threshold. This is in line with other research focusing on the effects of aerobic exercise.
When we look at the secondary outcome measures, we see that the clinically relevant improvements of the primary outcome (PCSS) were also seen on the Neck Disability Index, Headache Disability Inventory, Dizziness Handicap Inventory, neck pain and headache NPRS, and GROC. Here also, both groups improved.
The only between-group differences were observed in the objective measurements of cervical range of motion, cervical segmental pain of C0-C4, Flexion-Rotation test, and the Head Impulse Test. These differences were in favor of the experimental group performing cervicovestibular exercises on top of the aerobic exercise program. The vestibulo-oculomotor screening and vestibulo-ocular reflex were also improved in the intervention group only. These improvements however did not reflect in the subjective patient-reported outcome measures.
This trial delivered the treatments on a case-by-case basis, meaning they did not deliver a standardized set of exercises. The treatment was led by the findings of the baseline assessment. This is a plus, as it replicates real-life practice more closely.
Talk nerdy to me
The PCSS has been evaluated for internal consistency and has been found to have a moderate test-retest reliability of r = 0.65 over a 5.8-day test-retest interval. As the measurement moments were separated for over 3 weeks in between each moment, this may have had a spell on the outcomes. However, as the outcomes improved to such a major extent, it is unlikely that these differences not reflect true changes.
The control group participants more frequently received co-interventions compared to those in the intervention group. They also had higher symptomatology and frequency of symptoms.
As the study relied on patient outcomes and did not use specialized equipment, the results are applicable in physiotherapy practice. I would recommend limiting the number of questionnaires to fill in by the patient to the primary outcome of this study alone. The PCSS was used to calculate power and sample size. As your patient with a sustained concussion likely suffers from concentration difficulties, I would recommend avoiding overcomplicating the baseline assessment.
Take home messages
Aerobic exercise guided by the symptoms is the go-to treatment post-concussion. When the patient experiences neck pain and range of motion deficits, added cervicovestibular exercises may be of value. However, the addition of cervicovestibular exercises did not lead to larger improvements in the primary outcome PCSS. The results of this trial can be applied to use in practice, based on the findings of your baseline assessment, on a case-by-case basis.
Reference
Langevin P, Frémont P, Fait P, Dubé MO, Bertrand-Charette M, Roy JS. Cervicovestibular Rehabilitation in Adults with Mild Traumatic Brain Injury: A Randomized Clinical Trial. J Neurotrauma. 2022 Apr;39(7-8):487-496. doi: 10.1089/neu.2021.0508. PMID: 35102743. https://pubmed.ncbi.nlm.nih.gov/35102743/
Additional references
100% FREE HEADACHE HOME EXERCISE PROGRAM
Download this FREE home exercise program for your patients suffering from headaches. Just print it out and hand it to them for them to perform these exercises at home