Better Understanding of RCRSP: Assessment Guide for Physiotherapists

Introduction
Rotator cuff-related shoulder pain (RCRSP) is incredibly common in physiotherapy practice. Historically, papers relied heavily on terms like “subacromial impingement syndrome” and focused on specific orthopedic tests to pinpoint the problem. However, recent research has challenged the validity of those traditional ideas, since many asymptomatic individuals have structural abnormalities in their rotator cuffs, too, and surgeries aimed at “fixing” impingement aren’t consistently showing better outcomes than exercise or even placebo procedures. This leaves us with a crucial question: how should we be assessing and understanding RCRSP? Two important Delphi studies have suggested a shift towards looking at shoulder range of motion (ROM) and resisted movements (Littlewood et al. 2019 and Requejo-Salinas et al. 2022). We know that limited ROM and weakness are often present in RCRSP, but exactly how impaired they are and what they mean is still debated. Plus, there’s emerging evidence that pain patterns in the deltoid area might be a key indicator, and that myofascial trigger points (TrPs) could be contributing factors. Yet, solid data specifically mapping pain in RCRSP is lacking, and how it affects ROM, strength, pain, is still unknown. Therefore, this study was crucial to compare ROM, strength, pain patterns, and TrPs between people with RCRSP and those without, aiming to create a better understanding of RCRSP.
Methods
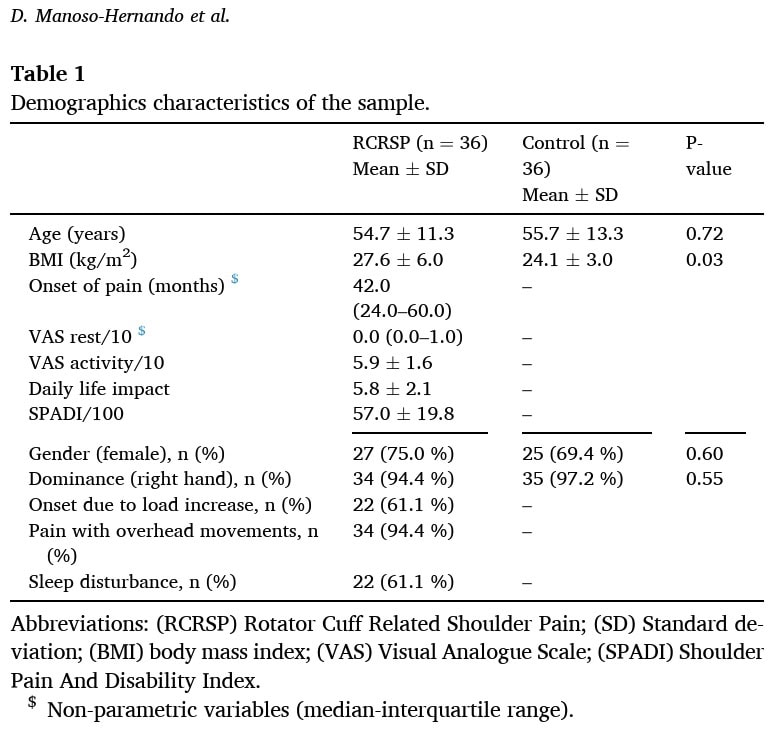
This study employed a cross-sectional, single-blinded design and included patients from the RCRSP waiting list at a Spanish hospital. The RCRSP patients were adults who were affected for at least 3 months, who were diagnosed by an orthopedic surgeon or a rehabilitation physician using a clinical examination and imaging findings. The RCRSP patients were matched with healthy and pain-free controls for age, sex, and dominant arm variables.
The Spanish version of the Shoulder Pain and Disability Index (SPADI) was filled in on the assessment day to describe pain characteristics from the RCRSP group. The VAS scale was used to describe the pain intensity at rest and with movement in the last week.
Before the physical examination took place, a standardized warming-up was provided to prepare the shoulder for clinical testing. The clinical testing included the following:
Range of motion (ROM) was assessed using a digital inclinometer:
- In a sitting position for active shoulder flexion and scaption
- Passive internal and external rotation ROM at 0°, 45°, and 90° of abduction were measured in supine
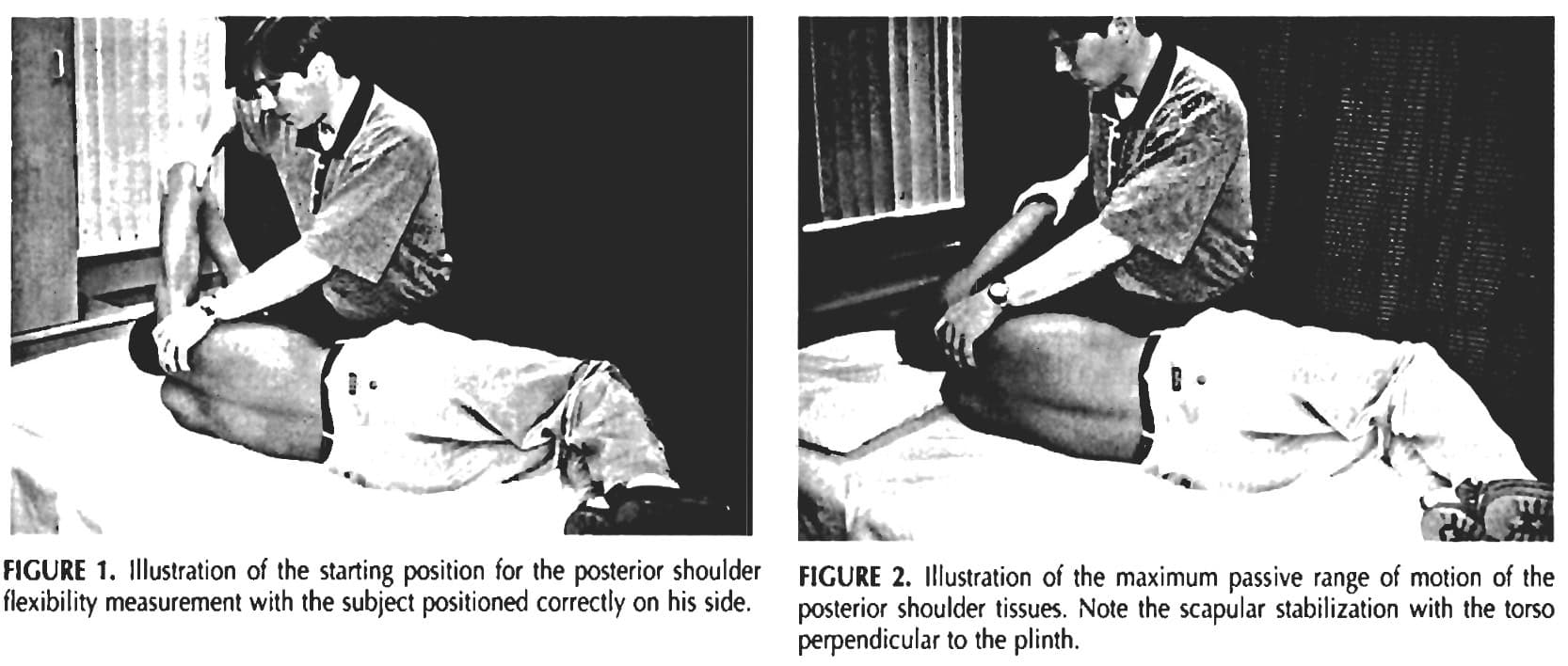
- Passive horizontal adduction ROM was assessed according to Tyler et al. (1999). Subjects lie on their sides on a plinth, humerus-length away from the edge, knees and hips bent at 90°, fully contacting the table, with acromions perpendicular and the non-tested arm under their head, keeping a neutral spine. The medial epicondyle is marked. The tester passively moves the humerus to 90° abduction, zero rotation, stabilizing the scapula in retraction. The humerus is then gently horizontally adducted until motion stops or humeral rotation occurs, indicating the end of posterior tissue flexibility. A 60cm carpenter’s square is placed perpendicular to the table next to the marked epicondyle, and the recorder marks the epicondyle’s inferior border level. The distance from the square’s bottom to the mark is measured in centimeters, with a greater distance indicating less flexibility and a shorter distance indicating more flexibility.
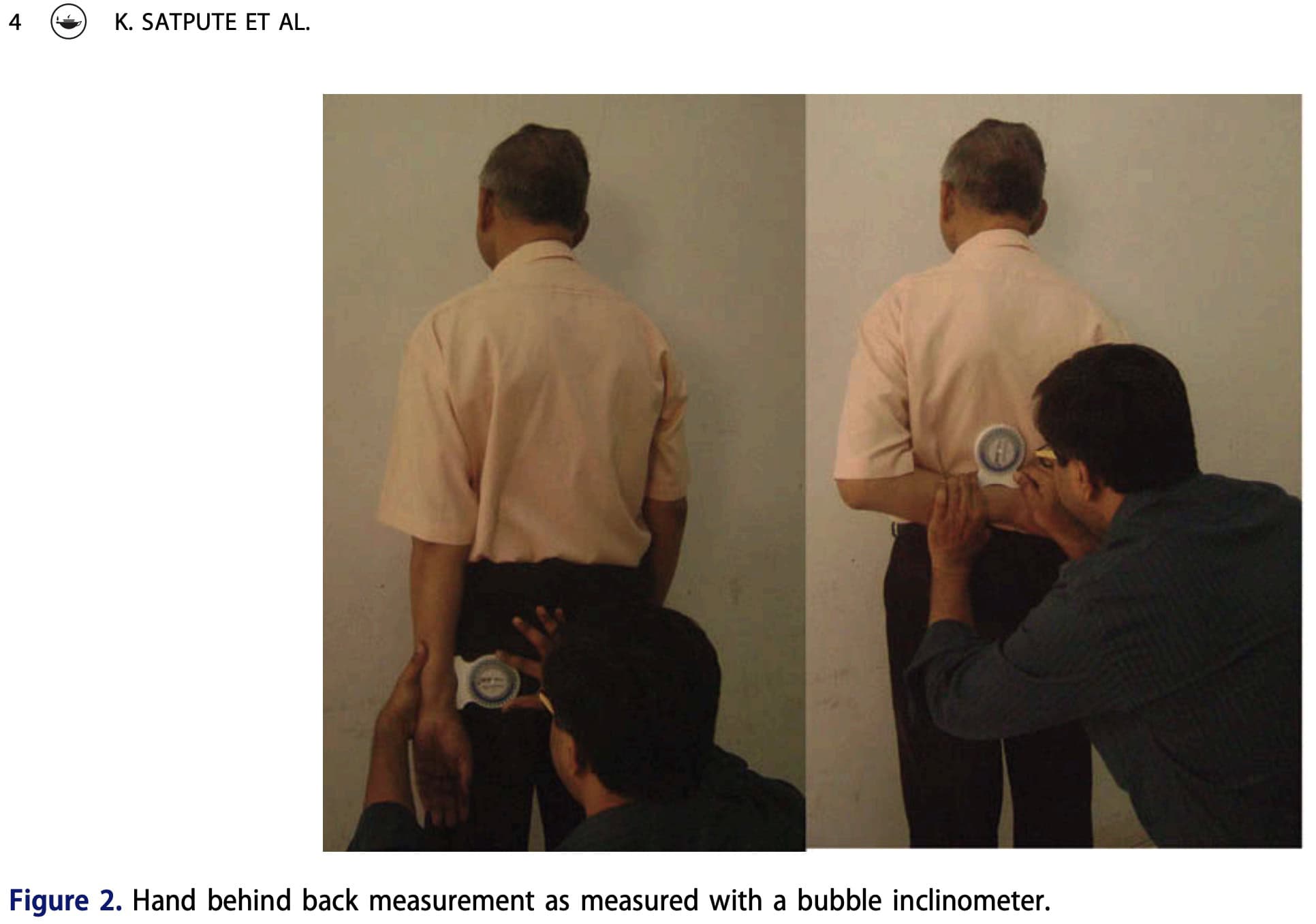
- The active hand behind back (HBB) position was measured according to Satpute et al. (2016). Standing, participants reached their hand behind their back as high as possible along their spine, keeping the back of their hand on their trunk and avoiding shoulder or spine movement. Their thumb’s highest point was measured. A bubble inclinometer on the radius determined ROM, with the movement ending at pain or maximal reach. Zero degrees of elbow flexion equaled no movement, while greater flexion indicated more ROM.
Strength was measured isometrically using a handheld dynamometer. The measurements were in the same position as their respective ROM assessments. Yet, strength for internal and external rotation was measured only at 0° and 90°. The mean of 3 5-second repetitions was measured using the “make” test, until limited by pain or weakness. Ten seconds of rest were allowed in between the 3 repetitions, and 3 minutes of rest were held in between positions.
Pain drawings were colored by the RCRSP patients on an electronic 3D chart with 4 different views. Their entire pain area was highlighted and colored.
Trigger points were assessed, according to the (1) presence of a palpable taut band in a skeletal muscle; (2) presence of a hyperirritable tender spot within the taut band; (3) local twitch response elicited by the snapping palpation of the taut band; and (4) presence of referred pain in response to TrP compression. The trigger points were classified as active, based on whether pressure application replicated the subject’s pain symptoms (localized and referred) and the subject recognized the pain, or latent if compression caused localized and referred pain but did not elicit symptoms recognized by the subject. The following muscles were assessed:
- Upper trapezius
- Supraspinatus
- Infraspinatus
- Teres minor
- Anterior deltoid
- Lateral deltoid
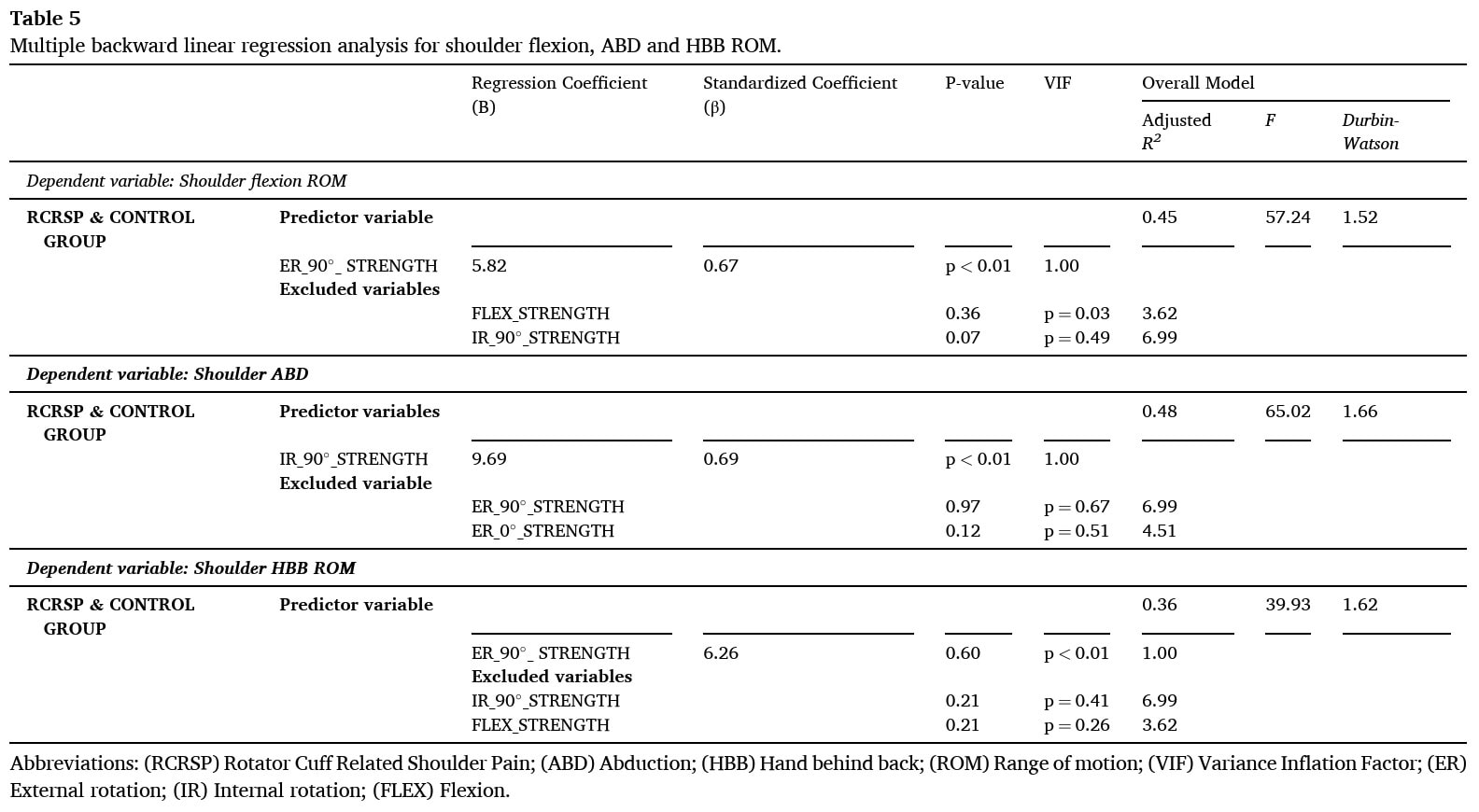
All the variables were compared between groups using independent t-tests and assessing effect sizes with Cohen’s d. Pearson’s correlation tests were conducted to analyze relationships between variables, and multiple backward linear regression models were used to determine the predictive capacity of shoulder strength on ROM variability, focusing on shoulder flexion, scaption, and HBB ROM.
Results
A total of 72 participants were included with equal numbers in both groups. The median onset of the RCRSP symptoms was 42 months (IQR: 24-60 months). There was a significant difference between the groups at baseline with regard to BMI.
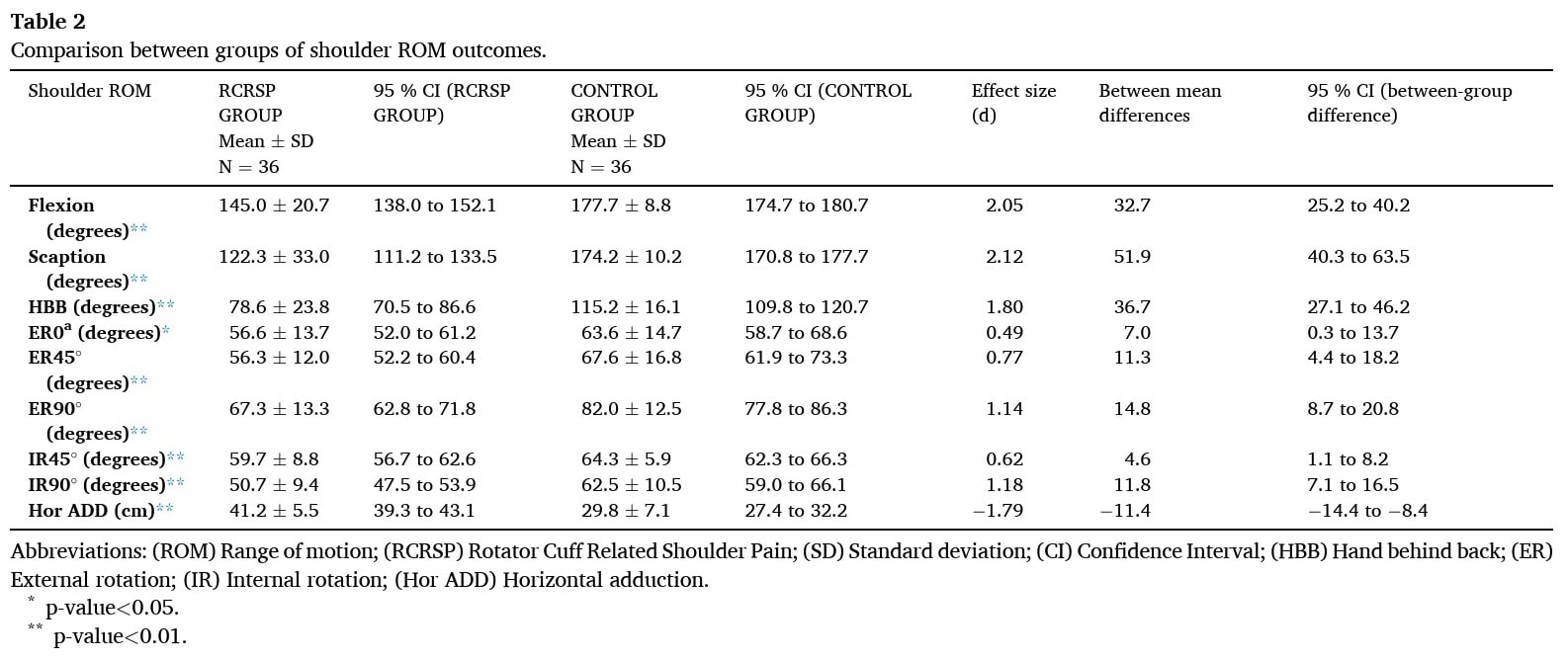
Compared to other groups, the RCRSP group showed significantly smaller shoulder ROM in several active and passive movements, including active flexion, scaption, and HBB; passive external and internal rotation at 90° abduction; and passive horizontal adduction, all with large effect sizes. At 45° abduction, passive external and internal rotation were also significantly smaller in the RCRSP group with a medium effect size. A significant difference with a small effect size was found for passive external rotation at 0° abduction.”
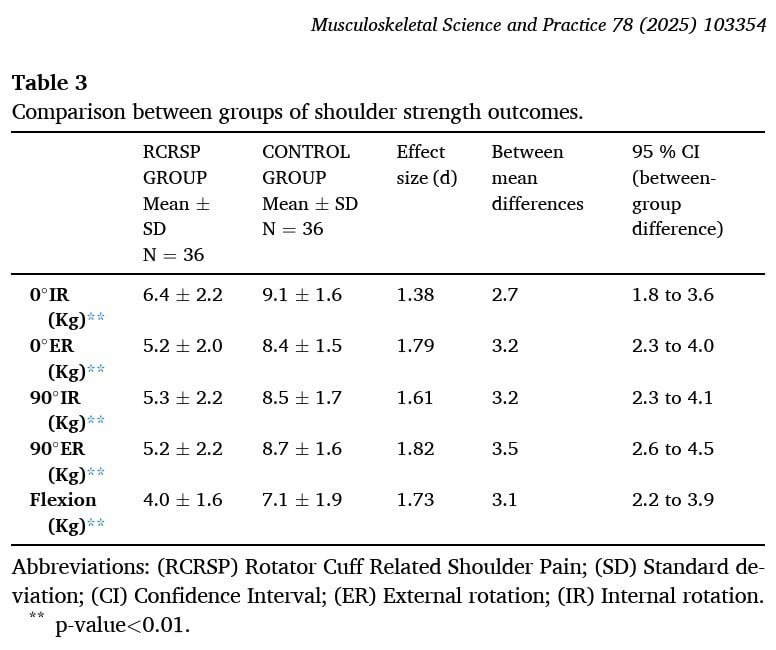
Significant differences with a large effect size were shown for internal and external rotation strength at 0° and 90° of shoulder abduction, and shoulder flexion.
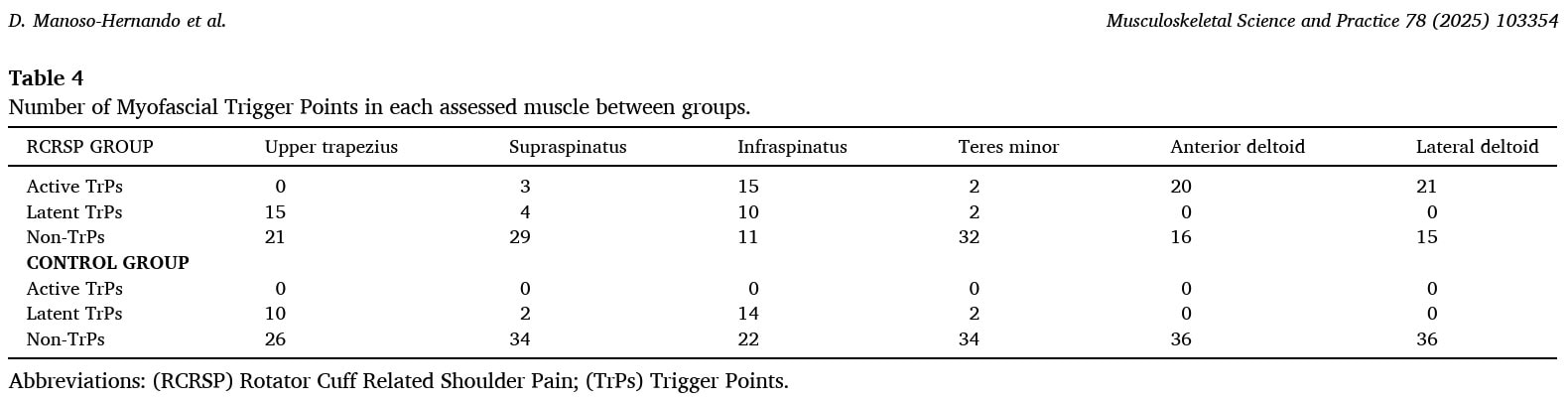
The RCRSP patients had a mean of 2.56 trigger points. They had active trigger points in a mean of 1.69 muscles, and 0.86 muscles with latent trigger points. The control group had only latent trigger points. Also, the total number of muscles with trigger points was significantly higher in the RCRSP patient group, but there was no difference in the number of latent trigger points between groups.
The most prevalent active trigger points were situated in the infraspinatus, anterior deltoid, and middle deltoid muscles.
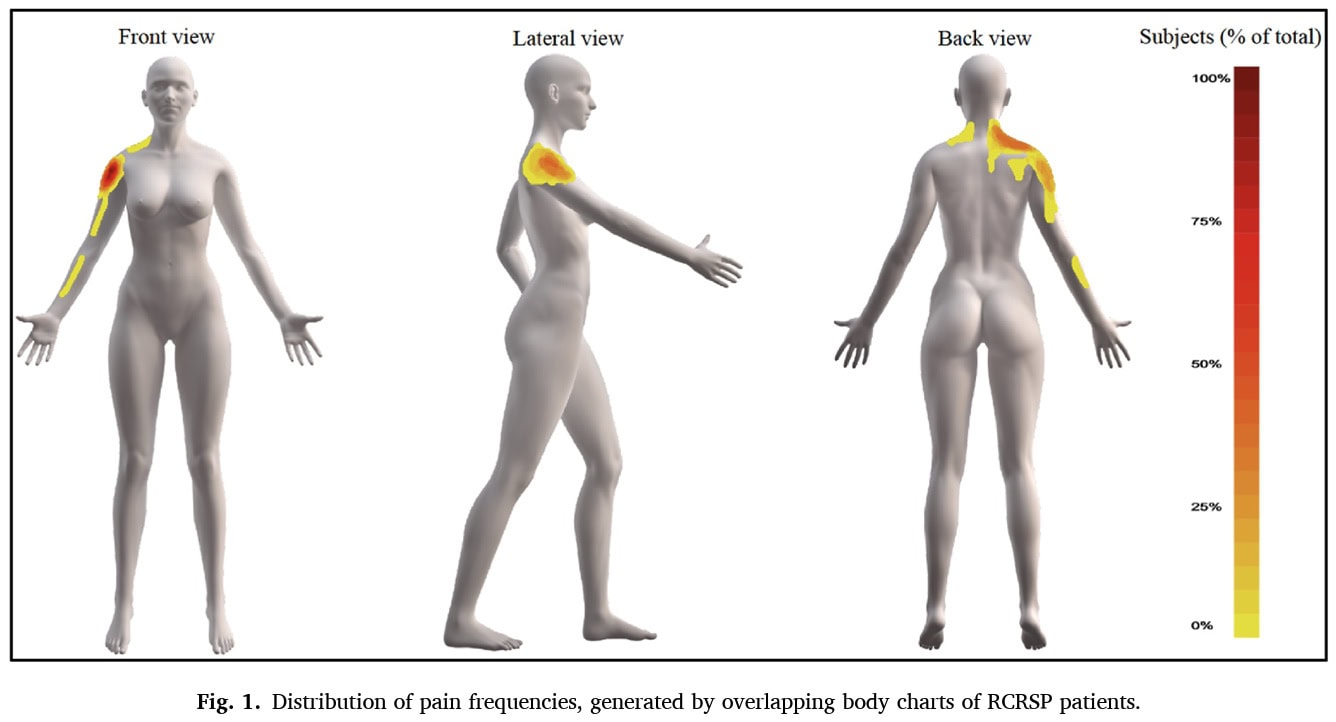
The pain frequency maps of the RCRSP group show the following pain distributions.
Regression analysis showed that external rotation strength at 90° was a significant predictor of active shoulder flexion ROM and active HBB ROM, while internal rotation strength at 90° was a significant predictor of shoulder abduction ROM (in the text, shoulder scaption was mentioned instead of abduction).
Questions and thoughts
It might look like a minor thing at first, but RCRSP patients were included in case they did not take any analgesic medication or NSAID within 48 hours of the examination. In clinical practice, you’ll often encounter patients who have already taken pain medications before consulting you, or who had received a trial of analgesic medication at symptom onset but no counseling or advice on activity modification, for example. We should also note that this population was in pain for a relatively long time, as the median of symptom onset was 42 months, ranging from 24 to 60 months. That’s 2 to 5 years! Pain medication is often adapted based on whether the pain is chronic or acute. These factors were not taken into account, and hence, to generalize the assessment recommendations to your practice, you could consider contacting patients before your consultation to discuss the possibility of not taking pain medications 48 hours before seeing you.
The study didn’t have a specific set of steps for dealing with pain during the strength test at 90 degrees of abduction. However, the way they handled pain during the range of motion tests suggests they knew pain could stop someone from moving fully. So, we can guess that if a person with RCRSP was in too much pain to get into or stay in the 90-degree abduction position for the strength test, the measurement would show that difficulty.
It is relevant to know that, in order to translate these results to your work field, patients with other shoulder conditions (glenohumeral instability/dislocation event, shoulder surgery in their medical history, frozen shoulder, severe arthritis, AC-joint dysfunction), cervical radiculopathy, systemic (e.g. diabetes) and neurological disorders were excluded. It was not specifically described how frozen shoulder was excluded, which seems important given the long nature of the symptoms these patients experienced. Despite that, by examining the tables, we see that the ROM limitations do not directly accord with those seen in frozen shoulder patients, although frozen shoulders also improve over time.
Talk nerdy to me
Nothing was mentioned about the imaging findings, which were required in the establishment of the RCRSP diagnosis. Were there different RCRSP entities (e.g. more bursal-related or more tear-related), and did findings of strength assessments and ROM differ between potential different entities? These different clinical entities were thus not considered in the analysis. Although imaging would not be necessary, it would have been informative to understand more of the imaging features used to diagnose the condition.
Participants were selected from a hospital waiting list, which may limit generalizability to the patients you see in practice. They were, however, not waitlisted for surgery. A broad spectrum of other conditions was excluded, but the authors acknowledge that people with neuropathic pain components could have been included since this was not screened for.
The cross-sectional design limits drawing causal associations, since the data was gathered from one specific moment in time. Nonetheless, it can tell us what variables are interlinked, in this case ROM and strength, but we can not derive the direction of the association between those variables. Furthermore, a lot of confounding variables can influence the associations. Like for example, pain during a certain movement could influence ROM and strength, but more than that may be happening, especially since we know that only 3 predicting variables were assessed. Another relevant finding was the baseline difference in BMI between the groups, which may also be confounding the effects.
Pain was measured for the average over the last week, which may be subject to recall bias. Furthermore, isometric strength, while indicative, is not a fully representative measure of true functionality. Weaknesses observed may be caused by pain, fear, arthrogenic muscle inhibition, etc. Trigger points were assessed by an experienced assessor, but nonetheless, this remains subjective. Are these true trigger points, or is there some guarding in those muscles, causing pain due to lowered pain pressure thresholds?
Take-home messages
External rotation strength at 90° of shoulder abduction was a significant predictor of how far someone could lift their arm forward. People with stronger external rotation at that specific angle tended to have better shoulder flexion ROM. Similarly, internal rotation strength at 90 degrees of shoulder abduction was a significant predictor of how far someone could lift their arm out to the side. Stronger internal rotation at that angle meant better scaption ROM. External rotation strength at 90 degrees of shoulder abduction explained a good portion of the variation in HBB ROM. In other words, a large part of how far someone could reach behind their back was linked to their external rotation strength at that angle. These findings can help in establishing a better understanding of RCRSP and effectively tailor treatments according to the identified impairments.
Reference
TWO MYTHS BUSTED & 3 KNOWLEDGE BOMBS FOR FREE
What university doesn’t tell you about shoulder impingement syndrome and scapula dyskinesis and how to massively level up your shoulder game without paying a single cent!