Feasibility of a six-month exercise intervention for patients with hip dysplasia: A mixed methods study

Introduction
Hip dysplasia, where the femoral head is not sufficiently covered by the acetabulum is a common finding in adults. It is more prevalent in those with hip pain and is associated with early osteoarthritis. Surgical options are available, but not for all. Contraindications are a body mass index above 25 kg/m2, being older than 45 years, and the presence of hip osteoarthritis. Some are not even willing to undergo surgery. Earlier investigations found good outcomes for patients following exercise and education. However, these trials did not include overweight patients or those with already evident hip osteoarthritis. Therefore, the evidence for exercise in this group not able to undergo surgery is nonexistent. Therefore, this trial examined the feasibility of 6-month exercise for hip dysplasia combined with education in this patient group.
Methods
This study was conducted to examine the feasibility of a 6-month exercise program with education in patients with hip dysplasia. To be eligible for inclusion, patients either had to be eligible for hip surgery but declined or were not eligible for surgery based on a negative impingement test, BMI >25, Tönnis hip osteoarthritis score >1, age >45 years, or reduced hip range of motion (<95◦ flexion and/or <30◦ abduction). Six patients were enrolled as part of a pilot study and received usual care for 3 months. This comprised information about self-management of hip symptoms and general advice on exercising and staying physically active.
Hereafter, 30 patients were included who followed the 6-month exercise for hip dysplasia. Eight sessions were completed in total of which the first two months consisted of 2 sessions per month and were followed by 4 sessions at a rate of 1 session per month. Advice on pain management, the importance of exercise adherence and progression, advice to lose weight if relevant, and advice on physical activity were given to the participants and were also visually supported. The 6-month exercise for hip dysplasia consisted of 4 exercises with 3 progression levels each. The four exercises that were performed were supine planks, side planks, squats, and single-leg standing balance exercises.
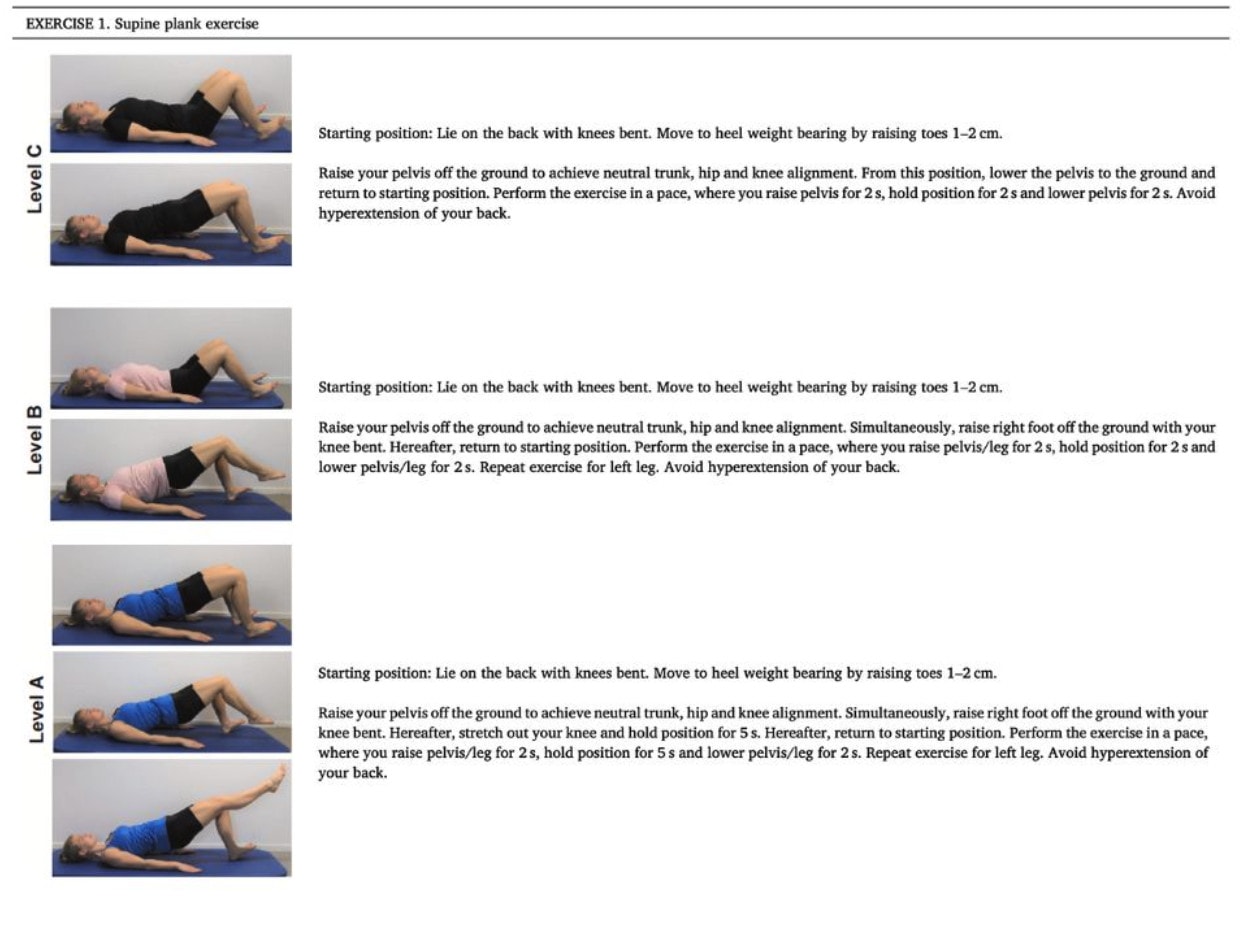
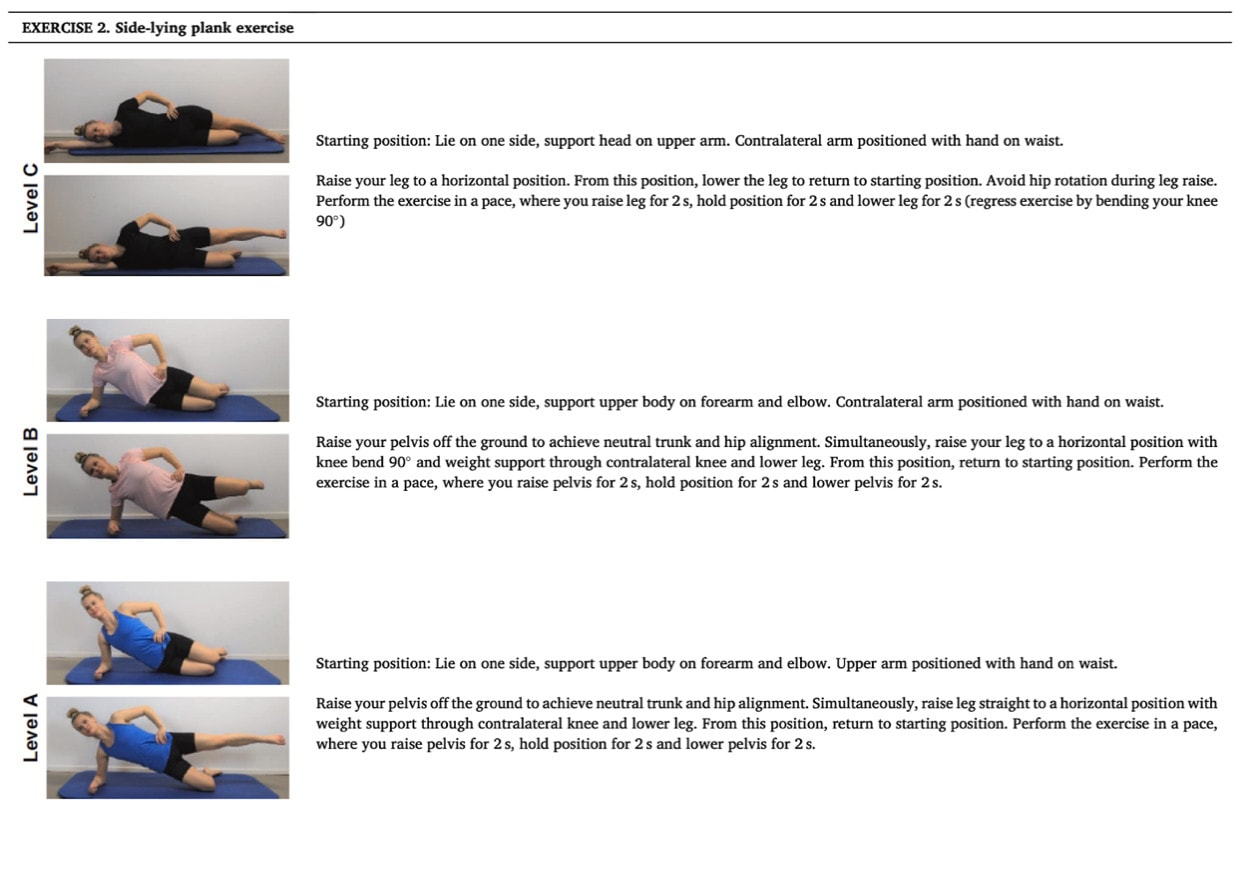
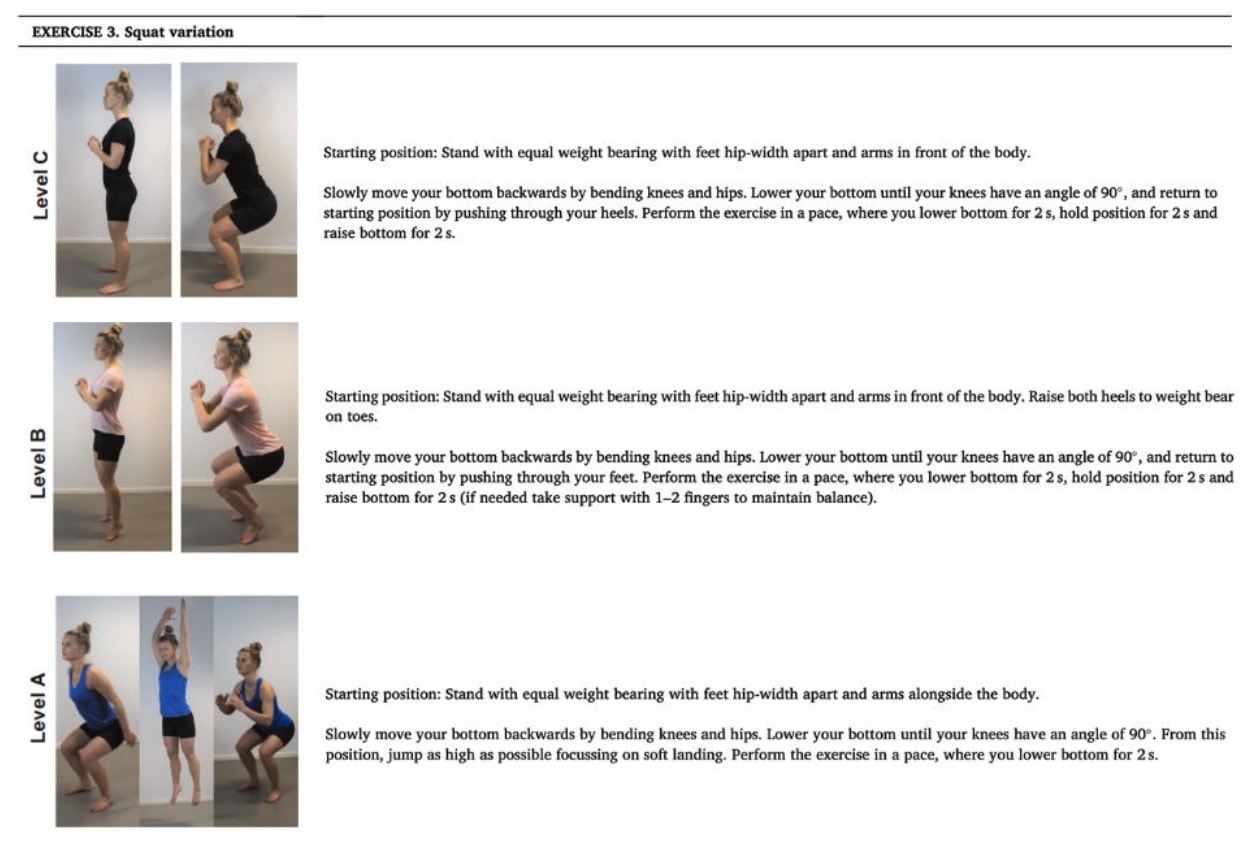
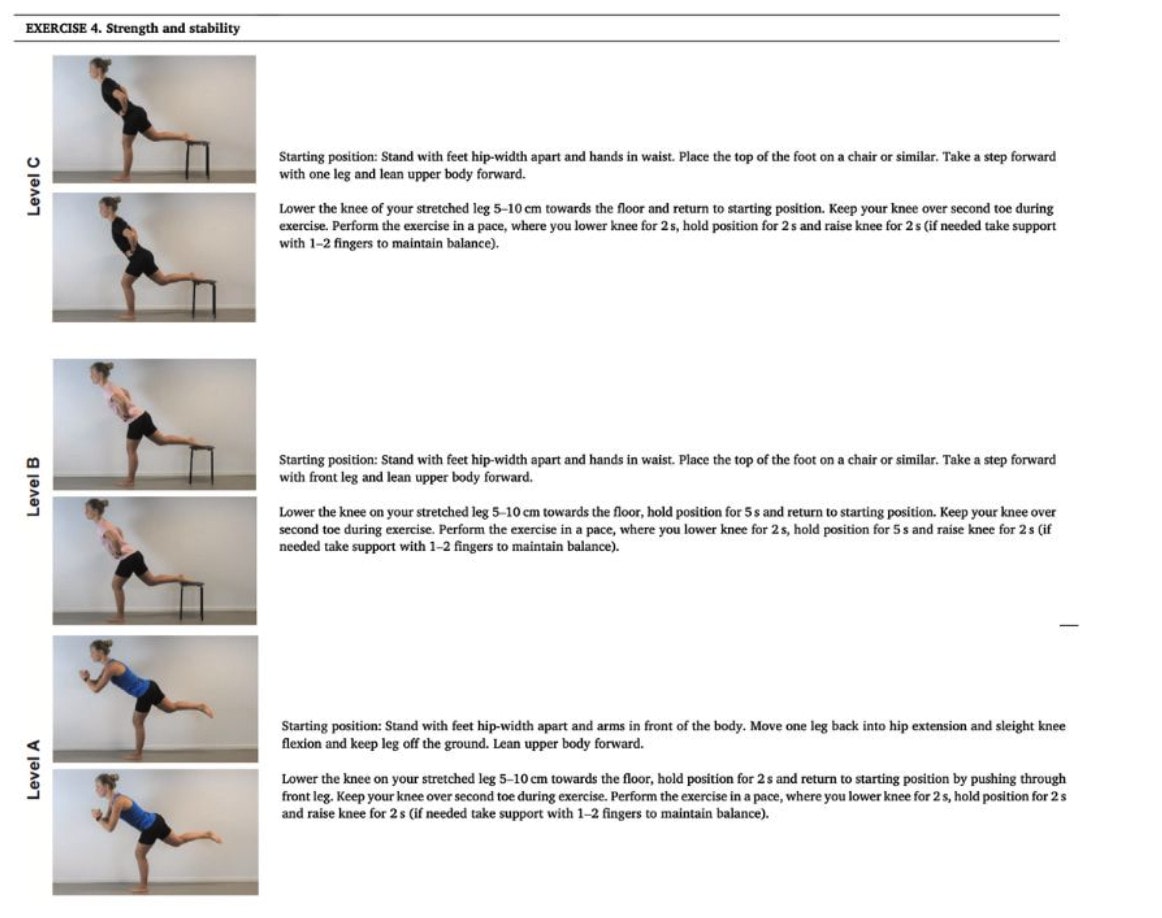
Everyone started with level C of each exercise and the purpose was to train at a level of perceived exertion from somewhat hard (level 5) to very hard (level 7) according to the Borg CR10 scale. In case participants could not progress to another level of difficulty, the number of repetitions performed was increased to 20.
Patient-reported outcomes were recorded with the Hip and Groin Outcome Score (HAGOS) on pain, symptoms, physical function, participation, and quality of life (scored 0–100, 100 best) from baseline to six-month follow-up. The study measured isometric hip strength in flexion, abduction, and extension with a dynamometer. Balance was measured with the Y-balance test and performance with the single-leg hop for distance. Minimal clinical relevance was defined as a change of more than 10 points on the HAGOS, >0.15Nm/kg in strength, >15cm on the Y-balance test, and >15cm on the hop for distance test.
Results
Thirty participants were recruited and 24 were available at the six-month follow-up. At 6 months clinically relevant improvements were found in the HAGOS pain, symptoms, and physical hip function. Further, the authors mention that significant improvements were found in all hip muscle tests and in the Y-balance test for all but 1 direction. Hip muscle strength improved with a mean difference of 0.18 Nm/kg in flexion, 0.20 NM/kg in abduction, and 0.25 Nm/kg in extension. The Y-balance test improved in each direction, and Table 3 does not reveal a non-significant direction of the Y-balance test, thus it is unsure which direction had not improved. The hop for distance test increased from 37 to 52 centimeters on average, which was significant and clinically relevant.
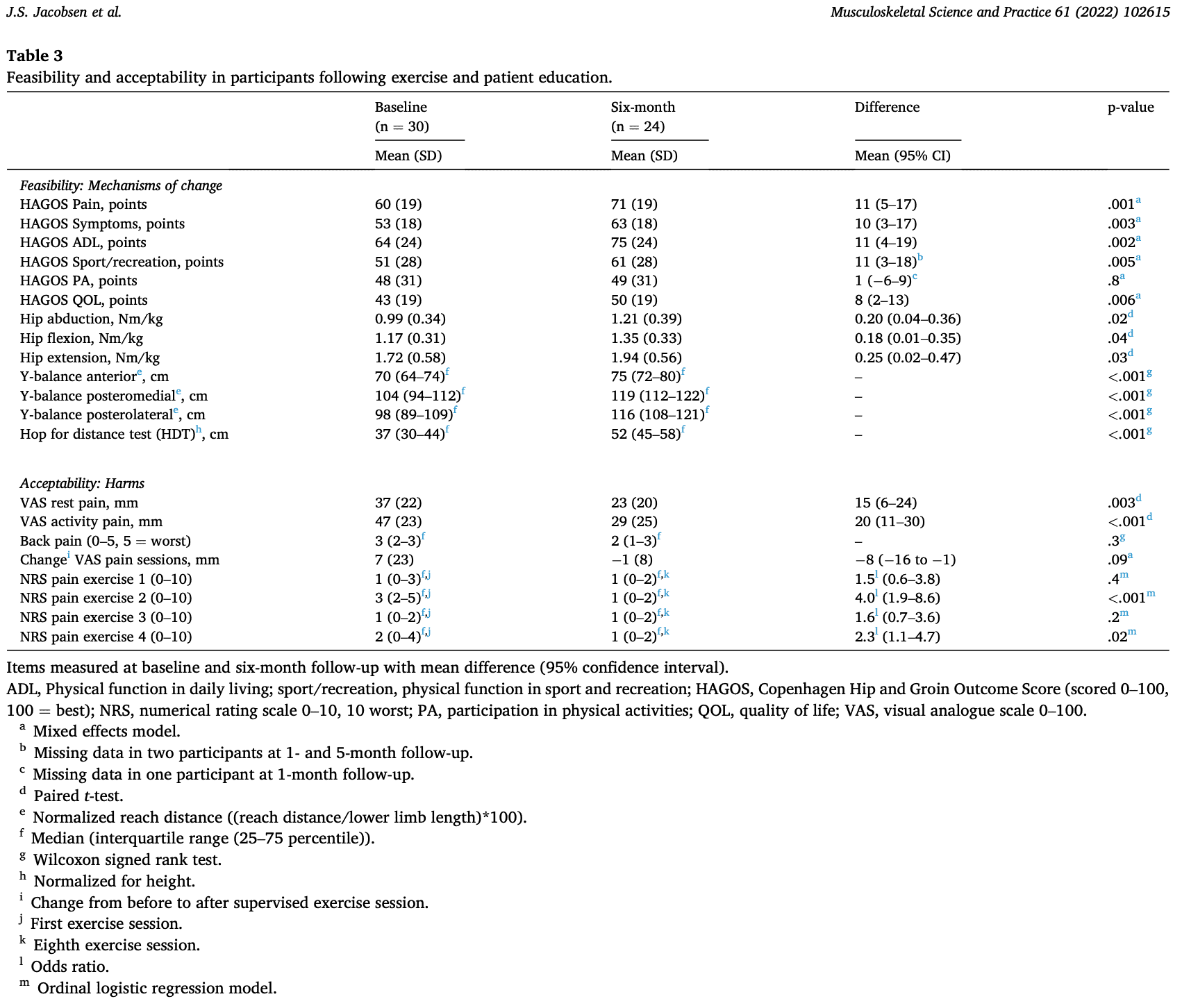
Clinically relevant improvements were found in 71% of individuals at 6 months for HAGOS pain. There was an important proportion of participants that could progress throughout the course of the study. 41%–73% of participants progressed to level B or higher levels in the four exercises after three months. This proportion increased to 75%–91% after six months, where 38%–58% also progressed to level A. Nineteen of the 24 participants achieved a 75% adherence.
Questions and thoughts
This review indicates that a program comprising 6-month exercise for hip dysplasia is feasible and safe. The participants achieved clinically relevant improvements in the defined outcomes. Without relying too heavily on these findings, this gives an indication of the possible benefits of such a program, but this has to be tested in more rigorous RCTs since the aim of this study was only to examine the feasibility and acceptability of 6-month exercise for hip dysplasia.
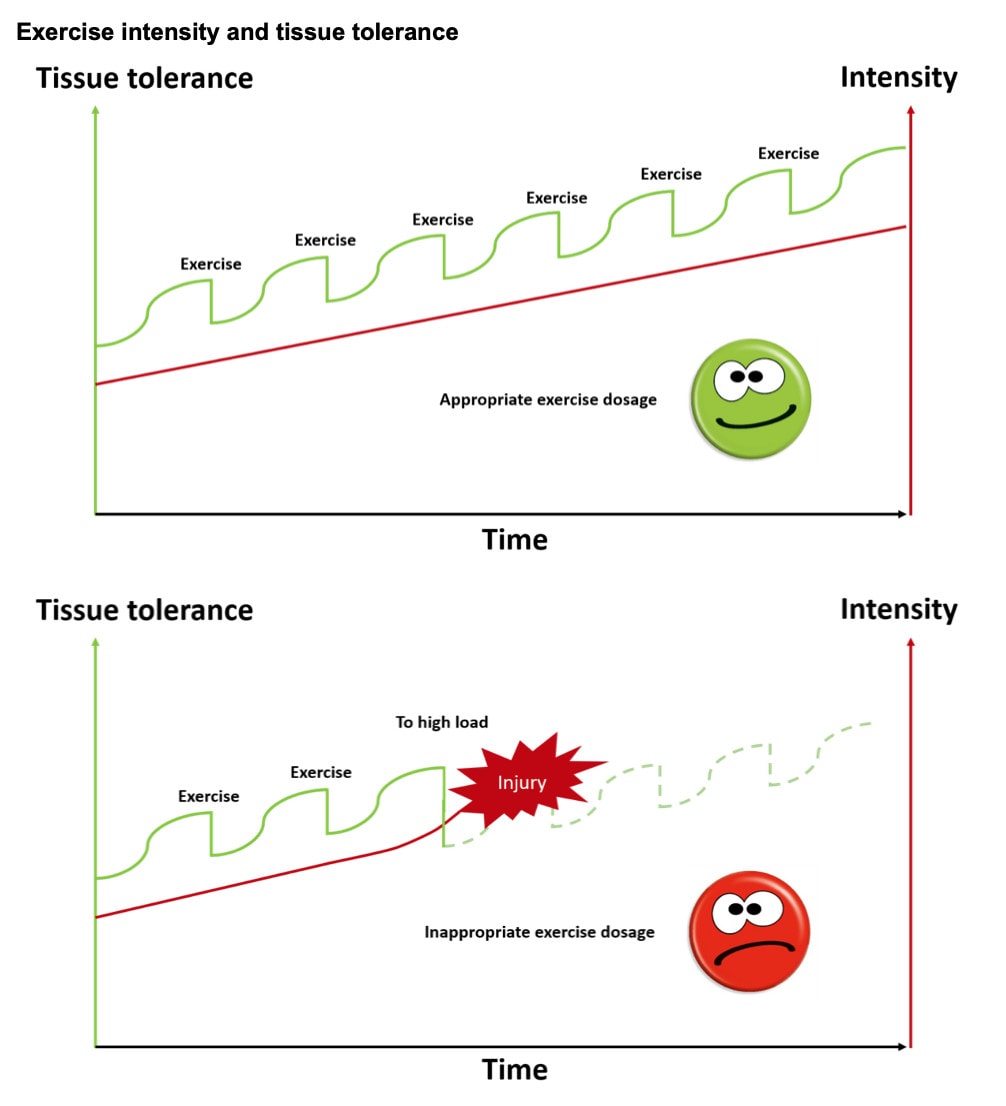
It was reported that patients could only progress to another exercise difficulty level during the supervised sessions. This was an adaptation of the original intervention but was deemed necessary as they found participants reporting minor exacerbations of hip pain and it was thought to arise from fast progression and incorrect performance of the exercises. This is an aspect to keep in mind, some patients will progress too quickly and this may lead to worsening of symptoms. It seems important to explain the importance of the balance between exercise intensity and tissue tolerance. In those patients who do not rely on balanced progressions, you can indeed allow them to make progressions when they are supervised only, rather than letting them make progressions at their own pace.
These exercise progressions may seem doable for us, but may be difficult for patients experiencing hip symptoms. Moreover, there are surgical options for patients with hip dysplasia, but these are not offered to patients with a BMI above 25 kg/m2 or aged more than 45 years. In these patients, the progressions may be difficult. This is not reflected in the included sample here as the average age was lower than 45 years. This sample had a median age of 30 years (IQR 24-41) and a median BMI of 24 (IQR 21-27). But the physical activity levels at baseline reveal that half of the sample was inactive or active below the recommended level of activity as defined by the WHO. They may have been less familiar with strengthening exercises and this may be one of the reasons why the progressions were difficult to make.
Talk nerdy to me
This feasibility trial recruited a convenience sample, thus, participants that were enthusiastic to participate or were close at hand, were recruited. This may have had a spell on the results, and in my opinion could have led to the high adherence to the program. However we do not know this for sure, a future RCT will give us more clarity about this. The relatively simple exercise program with only 4 exercises and 3 progression levels could also have led to the high adherence as the program probably wasn’t overwhelming to the participants.
The authors report clinically relevant improvements in HAGOS outcomes, and in the physical tests (strength, Y-balance and hop for distance). However, when inspecting table 4, it becomes clear that at 6 months only 62% of participants achieved an acceptable level of their symptoms, as reflected by the PASS. Even when 71% reported clinically relevant improvements in HAGOS pain scores, this doesn’t mean that all hip symptoms have vanished. This is an important aspect to keep in mind and communicate to your patient when he is following this rehab program. Participants with high baseline HAGOS pain scores (>80 points), meaning they had less severe pain, did not achieve (relevant) improvements. This is logical and may be explained by regression to the mean, where participants with low scores may improve more towards the mean. On the other hand, participants with already high scores do not have much room for improvement.
The title reveals that the 6-month exercise for hip dysplasia program also consisted of patient education. Yet, the prespecified progressions had to be changed so that they could only be made when supervised as many patients progressed too quickly and used incorrect technique, leading to exacerbations in hip pain. Two questions may be asked. Were the exercises and progressions poorly explained or was the education on when to progress the exercises not properly described? It seems that the patient’s education should be optimized in future trials to avoid this.
Take home messages
The 6-month exercise for hip dysplasia seems a relevant treatment option to offer patients. Although preliminary, it seems that the program leads to clinically relevant improvements in HAGOS outcomes and in hip flexor, abductor, and extensor strength and in the Y-balance test and performance on the hop for distance test. These outcomes should now be confirmed in an RCT, as this trial was a feasibility study.
Reference
LEVEL UP YOUR DIFFERENTIAL DIAGNOSIS IN RUNNING RELATED HIP PAIN - FOR FREE!
Don’t run the risk of missing out on potential red flags or ending up treating runners based on a wrong diagnosis! This webinar will prevent you to commit the same mistakes many therapists fall victim to!



