Thoracic Pain | Assesment & Treatment

Introduction & Epidemiology
Introduction
In contrast to the cervical and lumbar spine, less research is conducted on the thoracic spine. For this reason, Heneghan et al. (2016) called the thoracic spine the “Cinderella” region of the spine.
Clinically, thoracic spine pain occurs between the levels of C7-T1 and T12-L1 and is often, but not exclusively, associated with pathologies such as osteoporosis, osteoarthritis, Scheuermann’s disease, and ankylosing spondylitis (Briggs et al. 2009).
An increased thoracic kyphosis is often associated with “bad” posture. At the same time, this bad posture is commonly thought to be the reason for a patient’s pain experience. For this reason, we have aggregated studies that investigate the association between posture and pain and discuss the findings in the following video:
With all of this being said, there are certain situations in which posture and biomechanics matter more:
Epidemiology
Approximately 5% of patients referred to outpatient pain clinics suffer from thoracic pain (van Kleef et al. 2010). In a Danish study, a 1-year prevalence for thoracic pain of 13% was found in people between 20 and 71 years of age (Leboef-Yde et al. 2009). Another study by Briggs et al. (2009) describes a lifetime prevalence of thoracic pain between 3.7 to 77% with a higher prevalence in young adults and older females. They also report a 1-year prevalence ranging from 3 – 55% with most occupational groups having medians around 30%.
Roquelaure et al. (2014) looked at incidence rates of thoracic pain and found that 5.2 per 100 men and 10 per 100 women suffered from a new episode of thoracic pain. What was also striking is that thoracic spine pain was often associated with low back and neck pain.
Risk factors for the development of thoracic pain from the Roquelaure et al. (2014) study were older age (OR 6.0 for ≥50 years), being tall (OR 2.2), frequent/sustained trunk bending (OR 3.0), lack of recovery period or change in the task (OR 2.0) and driving vehicles (OR 2.8). In women, thoracic spinal pain was associated with a high perceived physical workload (OR 1.9). Surprisingly, being overweight or obese reduced the risk (OR 0.5).
No studies about the course of thoracic spinal pain or prognostic factors impeding or accelerating recovery have been published yet.
Diagnosis
Screening
Next to screening for general red flags like cancer, infections, fractures, and central neurological pathology, there are red flags that are specific to the thoracic region. Moreover, knowledge of specific pain syndromes in the thoracic area is important as (non-urgent) referrals to the GP or orthopedic specialist might be necessary for further treatment.
Fractures
For the thoracic region, the Supine Sign in combination with the Closed-Fist Percussion Test should be used to exclude a thoracic compression fracture.
Referred Visceral Pain
Thoracic Pain Syndromes
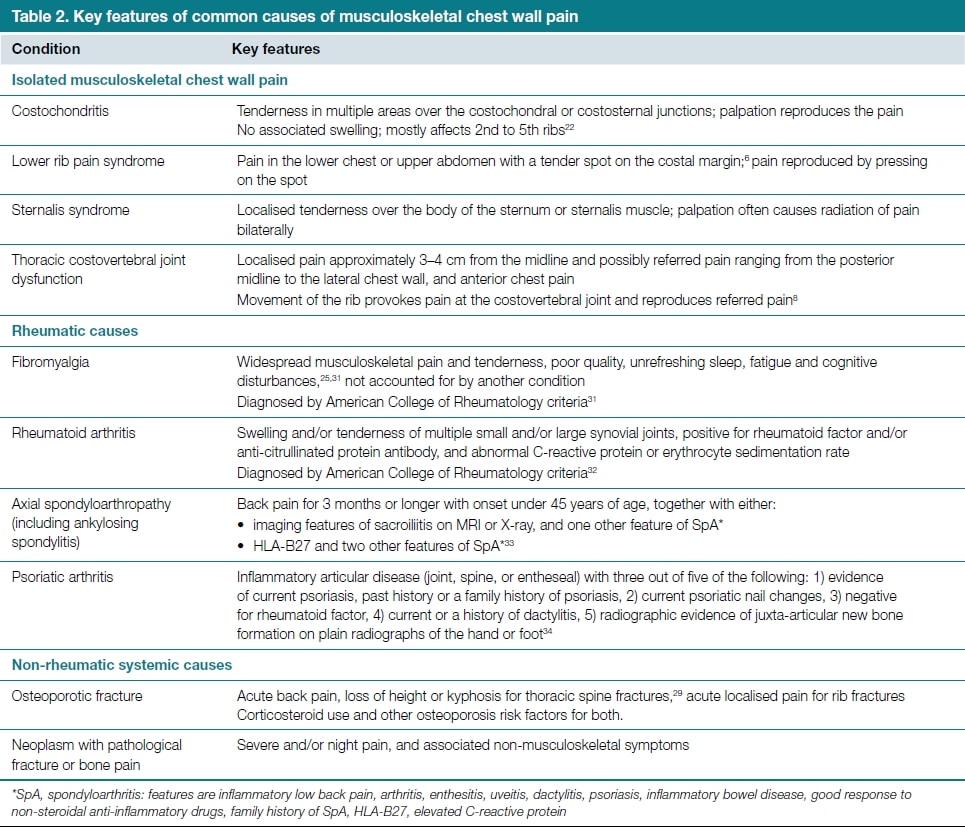
In patients with chest pain, the cause of pain may be benign in approximately 80% of cases, of which musculoskeletal chest pain accounts for almost 50% (Stockendahl et al. 2010). In the following we are presenting the clinical signs & symptoms of the most common musculoskeletal causes of chest pain (Winzenberg et al. 2015):
Next to asking for general and specific red flags, as well as different tracts that can cause referred pain to the thoracic area, you should always evaluate if the patient’s symptoms are influenced by movement. On top of that, a serious progressive course of the patient’s complaints might be another indicator of a serious underlying pathology, which makes a referral necessary.
Source of nociception
Anecdotally, the thoracic spine is considered a common source of anterior chest wall pain in patients presenting to general practice, although we are unaware of any incidence or prevalence data.
The innervation of the costovertebral joints suggests that pain in these joints could be referred to the anterior chest, but this has not been tested. The segmental referral patterns of the thoracic interspinous ligaments and paravertebral muscles (innervated by the posterior rami of the spinal nerves) have been investigated using injections of hypertonic saline, which has shown referral to the anterior, lateral, and posterior chest, and lower thoracic segments referring lower on the chest (Winzenberg et al. 2015).
Dreyfuss et al. (1994) evaluated pain referral patterns of the thoracic zygapophyseal joints from T3 to T11 in an asymptomatic population. They found that evoked referral patterns were consistent with a significant overlap with most thoracic regions sharing 3-5 different joint referral zones. The study provides preliminary evidence that the thoracic facet joints can be the source of local, as well as referred pain. The referred pain patterns looked as follows:
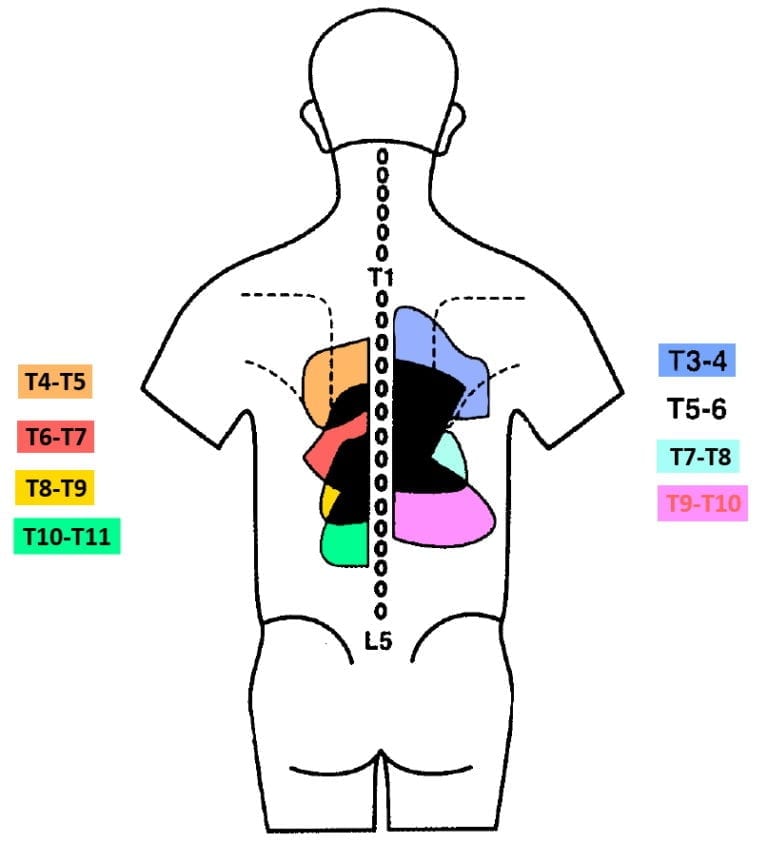
In all subjects, each joint caused the most intense area of evoked pain one segment inferior and slightly lateral to the joint injected. Thoracic zygapophyseal pain did not refer to more than 2.5 segments inferior to the joint injected, which differs from the cervical and lumbar region. Those two regions commonly have a more diffuse and broader pain referral. In the thoracic spine, no referral pain zones could be attributed to solely one facet joint. As the zygapophyseal joints are innervated by the medial branch of the dorsal ramus unilaterally, pain was only produced unilaterally and did not cross the midline. Anterior or lateral chest wall pain was not seen, although the authors argue that the pain referral zone might be broader in symptomatic subjects compared to asymptomatic subjects.
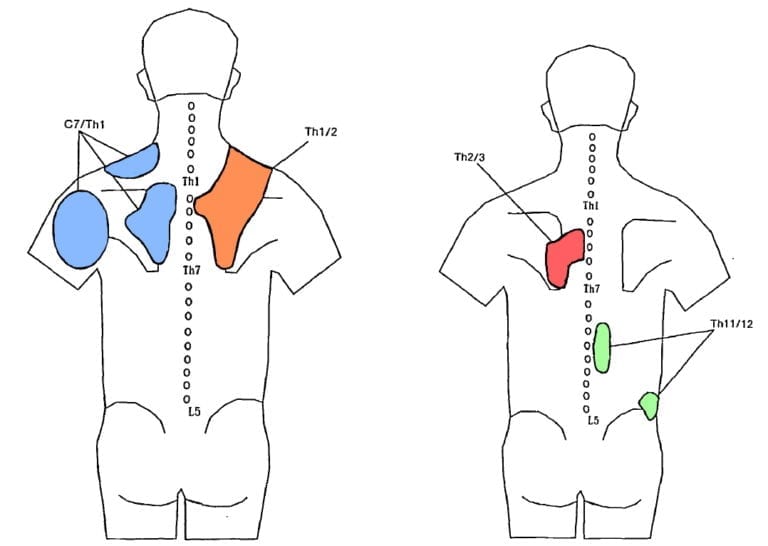
Fukuit et al. (1997) picked up the study by Dreyfuss et al. (1994) and examined the referred pain patterns for the cervicothoracic junction from C7-T1 down to T2-T3 and T11-T12 in patients with back pain. They add the following referred pain zones:
In contrast to the zygapophyseal joints, the costotransverse joints are innervated by the lateral branch of the dorsal ramus. Young et al. (2009) have therefore investigated the referred pain patterns for the costotransverse joints in asymptomatic volunteers. The authors found ipsilateral pain sensations which remained local to the targeted joint. Only pain from T2 injections appeared to refer to approximately 2 vertebral segments superior and inferior to the target joint.
Although pain referral maps can help approximate the location of nociception, all of the above-mentioned authors stress that pain referral patterns of the spine are insufficient in determining the exact source of nociception, because of their overlap.
To examine the segment of nociception, you can perform an intervertebral motion assessment in 3D extension for the upper thoracic spine to cause compression of the affected facet joints:
The mid and lower thoracic spine can be examined with the following technique:
For the costotransverse joints, the following techniques can be applied to exert stress on the joint capsules:
An alternative is to exert unilateral pressure from posterior to anterior direction (PA pressure) with the patient in prone position.
If the patient’s familiar pain is not reproduced during provocative testing, the source of nociception might not lie within the facet or costotransverse joints including their capsular apparatus.
Next to arthrogenic nociception, the examiner should consider local drivers of nociception such as myofascial structures that can be provoked by pressure, stretch, and contraction. As high pain intensity, wide-spread pain, and longer pain duration are all described as generic negative prognostic factors (Artus et al. 2017) in musculoskeletal conditions, knowledge about the source of nociception might enable the therapist to more specifically influence the patient’s pain experience during treatment.
Treatment
The thoracic area has been called the “Cinderella” region of the spine for a reason: there is no robust evidence in form of randomized controlled trials of physiotherapeutic interventions in patients with thoracic spinal pain. This means, that we will have to base our treatment approach entirely on the findings and prognostic factors we have found during patient history and assessment.
Heneghan et al. (2018) have shown that subjects who sit more than 7 hours a day and who are physically active for less than 150 minutes a week exhibit reduced thoracic mobility.
A review by Joshi et al. (2019) has found that increased thoracic kyphosis was positively correlated with the presence of forward head posture. Although thoracic mobility was reduced in the neck pain population, posture was not uniformly associated with neck pain and disability.
So while posture might not correlate with pain, literature shows that:
– It may be associated with psychological issues such as depression and chronic fatigue (Wilkes et al. 2017) and mental health is generally a negative prognostic factor for recovery in many musculoskeletal disorders.
– An increased kyphosis limits overhead mobility (Barrett et al. 2016) and may therefore limit your patient’s ability to carry out certain sports efficiently
In the following we will show you a mix of mobilization approaches and strengthening approaches that you can apply in practice:
Thoracic Mobilization
Aiken et al. (2013) present a case report about mobilization interventions in a patient with chronic thoracic pain. They used different mobilization techniques providing preliminary support for manual therapy in chronic thoracic pain. In the following, we will show you different MT and self-mobilization techniques for the upper, mid, and lower thoracic spine including the costotransverse and costovertebral joints. Similar to the neck region, the PIVM assessment techniques can also be used as treatment techniques. For treatment, make use of the Maitland mobilization grades I-IV according to your goal and patient’s reactivity.
Rib Mobilization
Thoracic Strengthening
Pagé et al. (2018) compared the stiffness in patients with thoracic pain to a healthy group. Surprisingly, the authors found a decrease in the global and terminal spinal stiffness in participants with thoracic pain compared to the healthy group. Pain intensity was only significantly and “moderately” correlated to spinal stiffness coefficients at one spinal level. We will cover this in more detail in the chapter on the lumbar spine, but it might be that pain does not automatically lead to an increase in muscle activity and stiffness. Anyhow, while spinal mobilization approaches might decrease pain via neurophysiological mechanisms, it might be necessary for some patients to try to increase stiffness. This can be achieved by strengthening exercises. An example of different exercises can be found here:
References
Goodman CC, Snyder TE. Differential diagnosis in physical therapy. WB Saunders company; 2000. (No direct link available)
Accredited online physiotherapy courses
- Built by the experts at Physiotutors
- Best price per CEUs/CPD Points
- Accredited in the Netherlands, Belgium, Germany, USA, UK, & Australia
- Learn anywhere, any time, and at your own pace!







