Low Back Pain | Assesment & Treatment

Learn
Physiotherapy for Low Back Pain | Assessment & Treatment
Prognosis & Course
Low back pain is aspecific in 90% of all cases. This means that no structural pathology can be detected as the source of back pain with the use of imaging techniques. In 10% of the cases, low back pain has a specific cause with about 1% linked to serious pathology (see screening). The other 9% are due to lumbosacral radicular syndrome, which is characterized by radicular pain in one leg with or without neurological symptoms.
Aspecific low back pain has a very favorable course:
- 90% of patients do not have to stay off work
- 75% of the remaining 10% are able to resume work within 4 weeks
A normal course is defined as an increase in activity and participation within the first 3weeks after the acute onset of low back pain so that limitations are minimal or nonexistent anymore. In an abnormal course, the patient is not able to increase the level of activity and participation or it even decreases within the first 3 weeks.
Screening & Patient History
Red flags are signs & symptoms that might indicate serious pathology. In the lumbar spine, the following specific red flags will have to be excluded before you can continue with your patient history-taking:
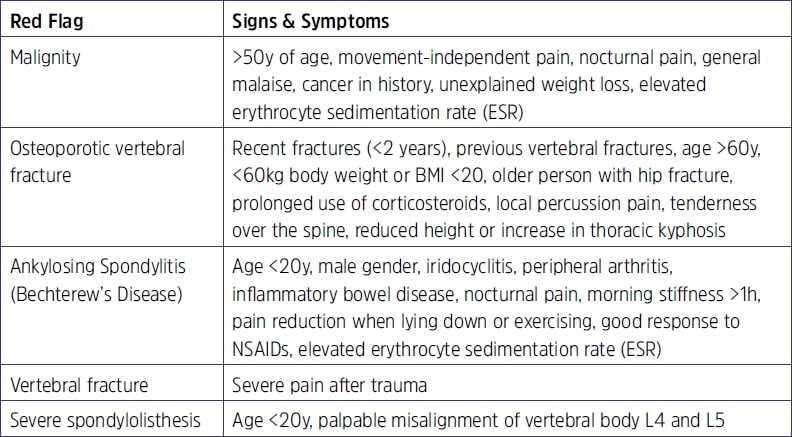
If you recognize a pattern or if you have a feeling of uncertainty, you should always refer the patient back to the general practitioner.
The guideline recommends using the NPRS or VAS scale to assess pain. For limitations in activity and participation, the PSC scale is recommended to assess patient-specific complaints.
In order to evaluate function, the guideline recommends the Quebec Back Pain DisabilityScale (QBPDS)
In case of recurring low back pain extra attention should be given to the following possible underlying causes of recurrence:
- Are there any changes in workload?
- Pressure of work?
- Activities involving body movements?
- Duration: Episodes of pain vs. pain-free episodes in-between
- Implementation of ergonomic recommendations?
- How is the patient’s compliance with earlier therapy?
Examination & Analysis
Like in other pathologies, your goal during the examination should be to test the hypothesis that you have formed during patient history-taking.
According to the guideline, the examination entails the following points regarding the thoracic, lumbar, and lumbosacral column, including the pelvis and the hip:
- Range of Motion (ROM), resistance, end-feel, pain, and possible radiation
- Muscles: length, end-feel, elasticity, tenderness upon stretch and contraction, muscle tone, coordination, and strength
- Skin: Level of grasp, shift, pliability, and end-feel
Performance of activities that were recorded in the PSCBased on your findings, you should be able to link the impairments in body function to the restriction that your patient experiences in activities and participation. If you suspect lumbosacral radicular syndrome, the guideline advises performing the straight leg raise test and the finger-to-floor distance (positive with a distance of 25cm during forward bending with straight knees). If you could exclude the presence of any red flags during your screening, as well as lumbosacral radicular syndrome, you can assume that your patient falls into the category of aspecific low back pain. Based on the whole diagnostic process, you should be able to place your patient into one of the following treatment profiles:

Treatment
Profile 1
- Reassure the patient• Explain that aspecific low back pain is not a serious condition, often resolves spontaneously, but may recur
- Advise your patient not to have bed rest and if bed rest is inevitable, the maximum number of days in bed should be 2
- Recommend a physically active lifestyle and explain that activity will not cause any damage to the back
- Advise your patient to slowly increase exercise and activity levels and to resume work as soon as possible as those measures promote healing
- N.B. Maximal number of treatment sessions should be 3!
Profile 2
- Same education and advice as in profile 1
- Prescribe exercise therapy
- If you suspect that the physical strain from work is impeding the recovery, an option is to contact the company’s GP if applicable
- If you suspect that impairments in body functions lead to the persistence of pain and limitations, manual therapy techniques like mobilizations and manipulations can beused
- If there is increased muscle tone, the guideline recommends limited use of passive treatment modalities like thermotherapy and massage (be careful as passive therapy shifts the patient’s locus of control to external)
- N.B. If treatment does not have an effect after 3 weeks, the patient’s GP should be contacted!
Profile 3
- Same approach as profile 1+2, but with more emphasis on information/advice and behavioral principles during the exercise program
- There might be a need for a multidisciplinary consultation and collaboration
- Design a graded activity program for the resumption or gradual extension of activities based on load rather than on the patient’s perceived pain level
- If the patient is on sick leave, the exercise should ideally resemble the targets forwork resumption
- Explain the negative influence of psychosocial factors on your patient’s recovery
- N.B. If treatment does not have an effect after 3-6 weeks, the patient’s GP should be contacted!
MASSIVELY IMPROVE YOUR KNOWLEDGE ABOUT LOW BACK PAIN FOR FREE
References
Accredited online physiotherapy courses
- Built by the experts at Physiotutors
- Best price per CEUs/CPD Points
- Accredited in the Netherlands, Belgium, Germany, USA, UK, & Australia
- Learn anywhere, any time, and at your own pace!







