Lumbar Radicular Syndrome

Body Chart
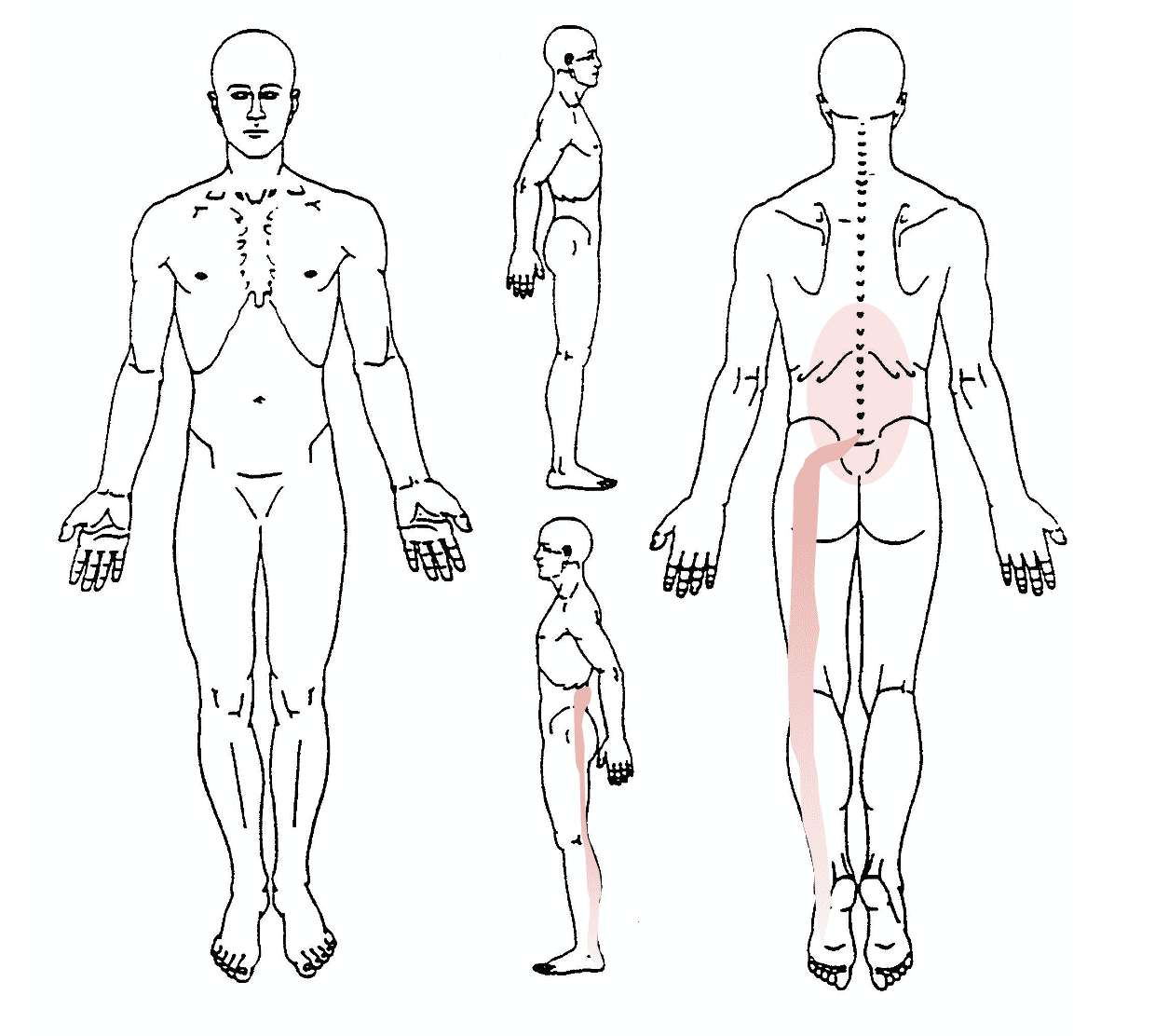
- Pain radiating into the lower extremity in a quasi-segmental but not dermatomal distribution
- Leg pain more than back pain
Background Information
Patient Profile
- 25 – 60 years old
Pathophysiology
Compression of nerve root within intervertebral foramen by tumor, HNP, vertebral body fracture or degenerative changes (e.g. stenosis through spondylophytes, spondylolysis, compression fracture)
Peripheral nociceptive pain. Local inflammatory response common. Central sensitization possible due to prolonged high levels of pain
Course
Constant (acute).
Mild compression has a good prognosis with physiotherapy. Severe paresis requires surgical intervention with subsequent physiotherapy. Within the first 6 months, significant improvement in QoL possible.
Psychosocial factors can negatively influence the prognosis.
Usually rather lengthy course with good prognosis if patient receives proper education, shows good compliance and does not have any yellow flags
History & Physical Examination
History
Insignificant trauma in history (twisting, lifting); possibly recurrent or at least history of less severe low back pain episodes
- Intense
- Deep
- Burning pain
- High intensity (acute) or varying intensity (subacute) VAS 5-10/10
- Tingling/numbness in lower extremity up to paresis
- More leg than back pain
- Central cord compression can lead to cauda equina syndrome
Physical Examination
Inspection
Relieving posture, typical shift or slight flexion
Functional Assessment
Pain apparent in all movement directions; significant increase with additional compression of the nerve; patient can provoke pain with ease; typically during transfers or apparent during gait (limping)
Passive Examination
PPIVMs & PPAVMs provoke pain on affected segment and segment above/below; stiffness and hypertonus of paraspinal structures; muscle length tests: Rectus femoris, glutei, iliopsoas…; in acute phase impossible due to pain
Special Testing
Neurodynamics
positive
Further Testing
Differential Diagnosis
- PEP
- Facetjoint hypomobility
- SI-Joint dysfunction
- coxarthrosis
- Spinal stenosis
Concerning cause of compression:
- Tumor
- Vertebral fracture
- HNP
- Spondylolisthesis
Treatment
Strategy
Decrease pain in acute phase. Move into pain-free directionsSubacute phase: coordination, strength, endurance, and stability of trunk.Patient education
Interventions
Acute:
- Treat surrounding structures and decrease compression
- Traction
- Movements into pain-free direction
- Infiltration
- Muscle relaxants/NSAIDs
Subacute:
- Trunk stability
- Motor control
- Neurodynamics
- Education on ergonomics
References
- Wiesner, R. and P. Westerhuis, Klinische Muster in der manuellen Therapie. Vol.2 2013: Thieme.
- Scaia, V., D. Baxter, and C. Cook, The pain provocation-based straight leg raise test for diagnosis of lumbar disc herniation, lumbar radiculopathy, and/or sciatica: a systematic review of clinical utility. J Back Musculoskelet Rehabil, 2012. 25(4): p.215-23.
- Tal-Akabi, A., Behinderung bei Rückenbeschwerden: Roland and Morris Disability Questionnaire (RMDQ), P. Oesch, Editor. 2010.
- Sullivan, M.J.L., Theoreticle perspectives on the relations between catastrophizing and pain, B. Thorn, Editor. 2001, The clinical journal of pain.
- Luomajoki, P.D.H., Artikel aus der Zeitschrift Physiopraxis: Wenn der Schmerz im Vordergrund steht. S2, Abschnitt: Angst vor Schmerzen nehmen.
- Hahne, A.J., et al., Outcomes and adverse events from physiotherapy functional restoration for lumbar disc herniation with associated radiculopathy. Disabil Rehabil, 2011. 33(17-18): p. 1537-47.
- K., B., The Quality of life of lumbar radiculopathy patients under conservative treatment, T.-T. S., Editor. 2009, Vajosanit pregl. p. 807-12.


