Migraine | Diagnosis & Treatment | All a physio needs to know

Physiotherapy for Migraines | Assessment & Treatment
Introduction & Epidemiology
The word “migraine is derived from the Greek word “hemikrania,” which was eventually translated into Latin as “hemigranea,” which was eventually translated to “migraine” in French. They are characterized by throbbing pain on one side of the head, a migraine is a moderate to severe headache.
Migraine attacks are intricate brain processes that frequently last from several hours to several days. Without an aura, migraines are most frequently encountered (75 percent of cases).
Additionally, a lot of people experience symptoms like feeling or being unwell, as well as increased sensitivity to light or sound.
Around 1 in 5 women and 1 in 15 men suffer from migraines, making it a widespread medical disease. Early adulthood is typically when they start.
Epidemiology
Stovner et al. (2007) found a lifetime prevalence of 14% for migraine. Migraines are about 3 times more prevalent in women compared to men. First episodes often start during puberty and prevalence increases until the ages of 35 to 39 before it decreases, especially after menopause (Lipton et al. 2007). In addition, it is ranked second in terms of the number of years people spend living with a handicap, after back pain.
When looking at the current prevalence of different forms of headaches, TTH is the most prevalent form in the adult population worldwide with a mean prevalence of 42%, followed by migraine with 11% (Stovner et al. (2007). The following graph shows the current prevalence of different forms of headaches in different age categories (Stovner et al. (2007):

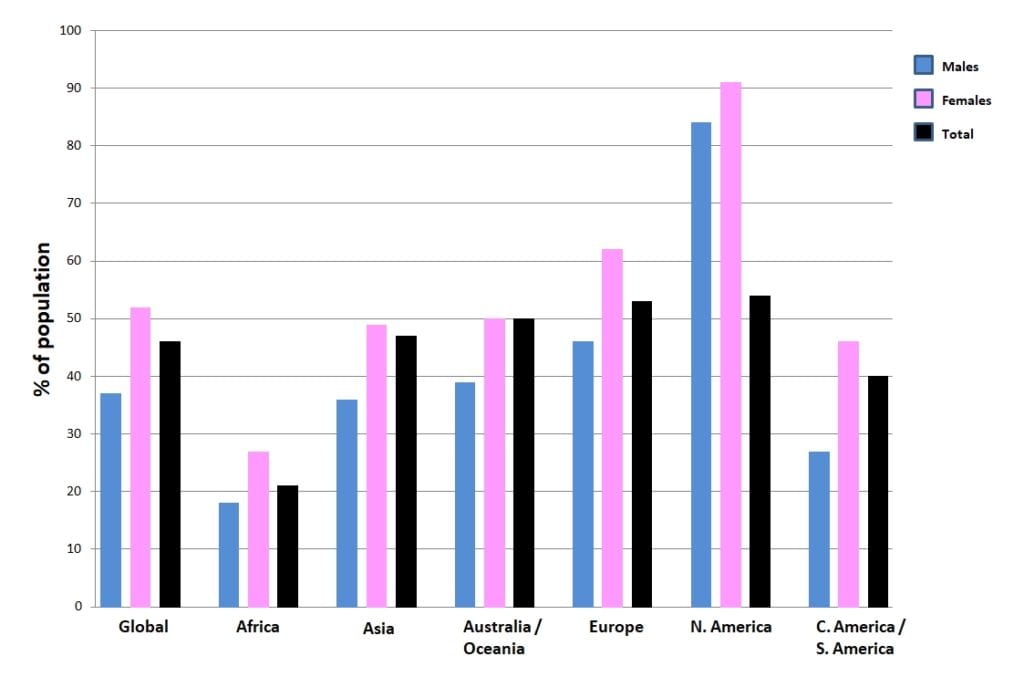
The following figure shows the prevalence of headaches on different continents around the world:
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Picture & Examination
The ICD-H III defines the following criteria to diagnose a migraine headache without aura:
Recurrent headache disorder manifesting in attacks lasting 4-72 hours. Typical characteristics of the headache are unilateral location, pulsating quality, moderate or severe intensity, aggravation by routine physical activity, and association with nausea and/or photophobia and phonophobia.
Diagnostic criteria:
A. At least five attacks1 fulfilling criteria B-D
B. Headache attacks lasting 4-72 hr (untreated or unsuccessfully treated)2;3
C. Headache has at least two of the following four characteristics:
1. unilateral location:
- pulsating quality
- moderate or severe pain intensity
- aggravation by or causing avoidance of routine physical activity (eg, walking or climbing stairs)
2. During headache at least one of the following:
-
- nausea and/or vomiting
- photophobia and phonophobia
Migraines with aura are defined as follows:
Recurrent attacks, lasting minutes, of unilateral fully-reversible visual, sensory or other central nervous system symptoms that usually develop gradually and are usually followed by headache and associated migraine symptoms.
Diagnostic criteria:
A. At least two attacks fulfilling criteria B and CB. One or more of the following fully reversible aura symptoms:
- visual
- sensory
- speech and/or language
- motor
- brainstem
- retinal
C. At least three of the following six characteristics:
- at least one aura symptom spreads gradually over ≥5 minutes
- two or more aura symptoms occur in succession
- each individual aura symptom lasts 5-60 minutes1
- at least one aura symptom is unilateral2
- at least one aura symptom is positive3
- the aura is accompanied, or followed within 60 minutes, by headache
D. Not better accounted for by another ICHD-3 diagnosis.
Examination
In comparison with healthy controls, migraineurs differ on provocation testing as well as neck endurance testing.
In comparison, Szikszay et al. (2019) conducted a systematic review and meta-analysis on the differences between MSK impairments in migraineurs and healthy people.
They recommend including testing for limited cervical ROM including the flexion-rotation test, forward head position, and pressure pain thresholds.
The goal of provocation tests is to recreate the patient’s familiar pain. This way, you are able to confirm the location of nociception in the cervical structures, possibly leading to referred pain to the head. While provocative testing for CGH can be done with the techniques shown in the following tab, the phenomenon of referred pain to the head for tension-type headaches and migraine can be provoked with the Watson test:
Although no clear cut-off values are given, the performance time can give an indication about neck flexor endurance:
Upper cervical range of motion in the direction of rotation can be reliably and accurately assessed with the Flexion-Rotation Test (Hall et al. 2010a, Ogince et al. 2007, Hall et al 2010b). This test – if positive – can give you an indication of limited rotation on segments C1/C2. In turn, hypomobility on C0/C1 or C2/C3 can lead to this limitation in rotation on C1/C2.So in case of a positive test, we still need to perform intervertebral motion assessment of all upper cervical segments in order to find the dysfunctional segment.
100% Free Headache Home Exercise Program
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
In the review and meta-analysis by Luedtke et al. (2016), it was found that sub-analyses of the different physiotherapy interventions showed that aerobic exercise and a combination of physical and psychological interventions were effective for the reduction of migraine attack duration; however, no trials were available that used either manual therapy, trigger point therapy, or strength training. In their systematic review and meta-analysis, Lemmens et al. (2019) confirm that aerobic exercise seems to be able to reduce migraine frequency with a mean reduction of 0.6 ± 0.3 migraine days/month. Krøll et al. (2018) investigated the effects of aerobic exercise in migraineurs with concomitant TTH and neck pain and found that exercise reduced migraine frequency, pain intensity, and duration pre and post-intervention. However, compared to the control group, the results did not reach significance.
In the case that neck endurance is reduced, you might want to try the following exercise program:
References
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Finally Learn how to Diagnose & Treat Patients with Headaches


What customers have to say about this online course
- Robbert Alblas13/09/24Headache Treatment in Clinical Practice Great insights
Very useful evidence based information. I do think this would be better if he would talk in his own language.Barry de Wit17/08/24Headache Treatment in Clinical Practice Review Headache Treatment in Clinical Practice
De cursus is erg duidelijk. Ook zijn de instructievideos wat betreft de tests en behandelingen erg nuttig om in de praktijk toe te passen! - Broes de Landsheer10/05/24Headache Treatment in Clinical Practice REVIEW COURSE HEADACHE
Iets te wetenschappelijk. Er worden heel veel artikels gegeven die je moet lezen en zo kom je aan het aantal uren studietijd. De video’s zijn echter zeer beknopt. Er worden ook geen slides gegeven van de video’s (je hebt dus geen naslagwerk).
Weinig praktisch toepasbaar vond ik.
Comment Physiotutors: Wij hebben inmiddels alle slides toegevoegdGoswin Arts-Opdam10/05/24Headache Treatment in Clinical Practice HEADACHE TREATMENT IN CLINICAL PRACTICE
Erg fijne en duidelijke cursus. Je krijgt genoeg handvatten mee en daarna kan je zelf bepalen welke je toepast in de praktijk. Ik kan patiënten met verschillende hoofdpijn nu in elk geval beter helpen. - Beppeke Molenaar14/04/24Headache Treatment in Clinical Practice OVERALL A GREAT COURSE
Great course, very informative.Tessa van der Zanden26/03/24Headache Treatment in Clinical Practice GOED TOEPASBARE CURSUS
Cursus die gelijk goed toepasbaar is in de praktijk. De Nederlandse ondertiteling is erg fijn. Goede balans tussen theorie en praktijk. Makkelijk in eigen tijd in te plannen en uit te voeren. - Bart de Ruijter20/03/24Headache Treatment in Clinical Practice LEUKE TOEPASSELIJKE CURSUS
Leuke toepasselijke cursus, nu ook vertaald in het Nederlands, wat het makkelijker maakt.
Filmpjes zijn wel in Engels, maar ondertiteling aan is een optie.
Goede combinatie van theorie, wetenschap en praktische handvaten.
Zeker een aanrader.Peter Tuyp27/02/24Headache Treatment in Clinical Practice GOOD COURSE
Good course, easy to follow.
Knowledge up to date after course. - Harmen van Delft25/02/24Headache Treatment in Clinical Practice INSTRUCTIEVE HOOFDPIJN CURSUS
de theoretische achtergrond en praktische vaardigheden zijn goed gecombineerd en bruikbaar in de praktijk.Laura Bradshaw05/02/24Headache Treatment in Clinical Practice GREAT CONTENT AND RESOURSES
The course was full of explanations, plenty of research and demonstrations. I would say that it took me longer than 14 hours to complete as I wanted to be thorough with my reading and practical component.
Rene and the physio tutors team were always available via email if you needed any info.
I would recommend this course if you want a better understanding of the management and manual therapy of headache and migraine. - Jelter Wahlen03/12/23Headache Treatment in Clinical Practice GREAT COURSE!
Great course to update your knowledge about headaches.
Evidence based and easy to implement in practice!Max Dienemann09/10/23Headache Treatment in Clinical Practice TOP
Great course! Everything is covered from diagnosis to treatment (-options) including the latest evidence backing everything up. The practical/skills videos on are also perfectly explained, therefore hands on skills and exercises can be easily implemented in daily practice. - Danitsja Wendt11/09/23Headache Treatment in Clinical Practice UITGEBREIDE HOOFDPIJNCURSUS
Veel informatie over de drie meest voorkomende hoofdpijnsoorten. Eerst uitgebreid theoretische achtergrond.
Daarna ook veel aandacht voor onderzoeken en behandelingen, verduidelijkt met filmpjes.
Fijn dat deze informatie ten alle tijden teruggekeken kan worden voor een opfrisser.
De cursus zelf is vertaald in het Nederlands, maar de vele wetenschappelijke artikelen zijn dat helaas niet.
Hierdoor ging bij mij wel erg veel tijd zitten in het doornemen daarvan.
Comment Physiotutors: All scientific literature is in English. That is a reality that we cannot change.Willem Nijssen31/07/23Headache Treatment in Clinical Practice GOOD QUALITY COURSE WITH UP-TO-DATE LITERATURE
The course is well structured and with up-to-date literature. It provides enough practical tips. There’s definitely a lot to learn about this subject! - Jesse de Louw11/07/23Headache Treatment in Clinical Practice GOOD COURSE
Good EBP study, with a nice variety of information. Sometimes a little bit hard to follow the information given in another language than my own. (Comment Physiotutors: This customer probably did not see the option to switch to Dutch)Hamad Alkahtani16/06/23Headache Treatment in Clinical Practice Very Interesting info and practical knowledge - M.A.G. Kuipers15/06/23Headache Treatment in Clinical Practice INFORMATIEVE CURSUS MBT HOOFDPIJN
Goede cursus, helaas niet in Nederlands en helaas zijn ook niet alle artikelen makkelijk te verkrijgen
duidelijke filmpjes met goede technieken mbt onderzoek en behandeling
Opmerking Physiotutors: De gehele cursus is wel in het Nederlands verkrijgbaar.Lennart Kroes17/04/23Headache Treatment in Clinical Practice A PERFECT COURSE TO UPDATE YOUR KNOWLEDGE ABOUT HEADACHE
Evidence-based, easy to follow. Perfect! - Erik Swarts09/03/23Headache Treatment in Clinical Practice GREAT COURSE!
First time doing a Physiotutors course. great way to learn on a high level of evidence. You can watch and rewatch everything for as long as you want before you take the exam.Daniel Klimsa31/01/23Headache Treatment in Clinical Practice GREAT COURSE!
Well-structured course with lots of evidence-based material.
Theory is well explained and you get a lot of additional reading material.
I would like to see improved quality of the explanations in the video portion of the course.