Lateral Ankle Sprain | Diagnosis & Treatment

Lateral Ankle Sprain | Diagnosis & Treatment
As a clinician, you have likely seen your fair share of patients with lateral ankle sprains. But how confident are you in your ability to accurately diagnose and effectively treat this common injury? In this post, we’ll delve into the latest research on lateral ankle sprains, including risk factors that can contribute to their development, diagnostic tools to help differentiate between various types of ankle injuries and evidence-based treatment options that can promote optimal healing and prevent future recurrences. Whether you’re a seasoned sports medicine specialist or a primary care physician who sees occasional ankle injuries, this post will provide valuable insights and practical tips for managing this all-too-common condition.
Pathomechanism
Sudden rapid inversion and internal rotation that will load the lateral ligaments of the ankle is the common mechanism. Other possibilities are a medial to lateral directed external force to the leg while planted or just before planting, or forced plantar flexion in for example a blocked kick (Andersen et al. 2004). Landing after a jump is another mechanism to consider. Oftentimes a ‘bad landing’ is blamed but this is not always the case (Bagehorn et al. 2023).
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Presentation & Examination
Risk factors
Vuurberg et al (2018) described several risk factors:
Intrinsic:
- Limited dorsiflexion ROM
- Reduced proprioception
- Reduced preseason deficiencies in postural control (positive single-leg balance test)
- BMI (high and/or low, depending on the source)
- High medial plantar pressures during running
- Reduced strength
- Reduced coordination
- Reduced cardio respiratory endurance
- Limited overall ankle joint ROM
- Decreased peroneal reaction time
- Females > males
- Previous ankle injury (although results are conflicting)
Extrinsic:
- Sport: aeroball, basketball, indoor volleyball, field sports, climbing
- Lots of jumping and landing in volleyball
- Playing soccer on natural grass
- Soccer defender
- High heels
- Competition risk is higher in boys compared to girls
History
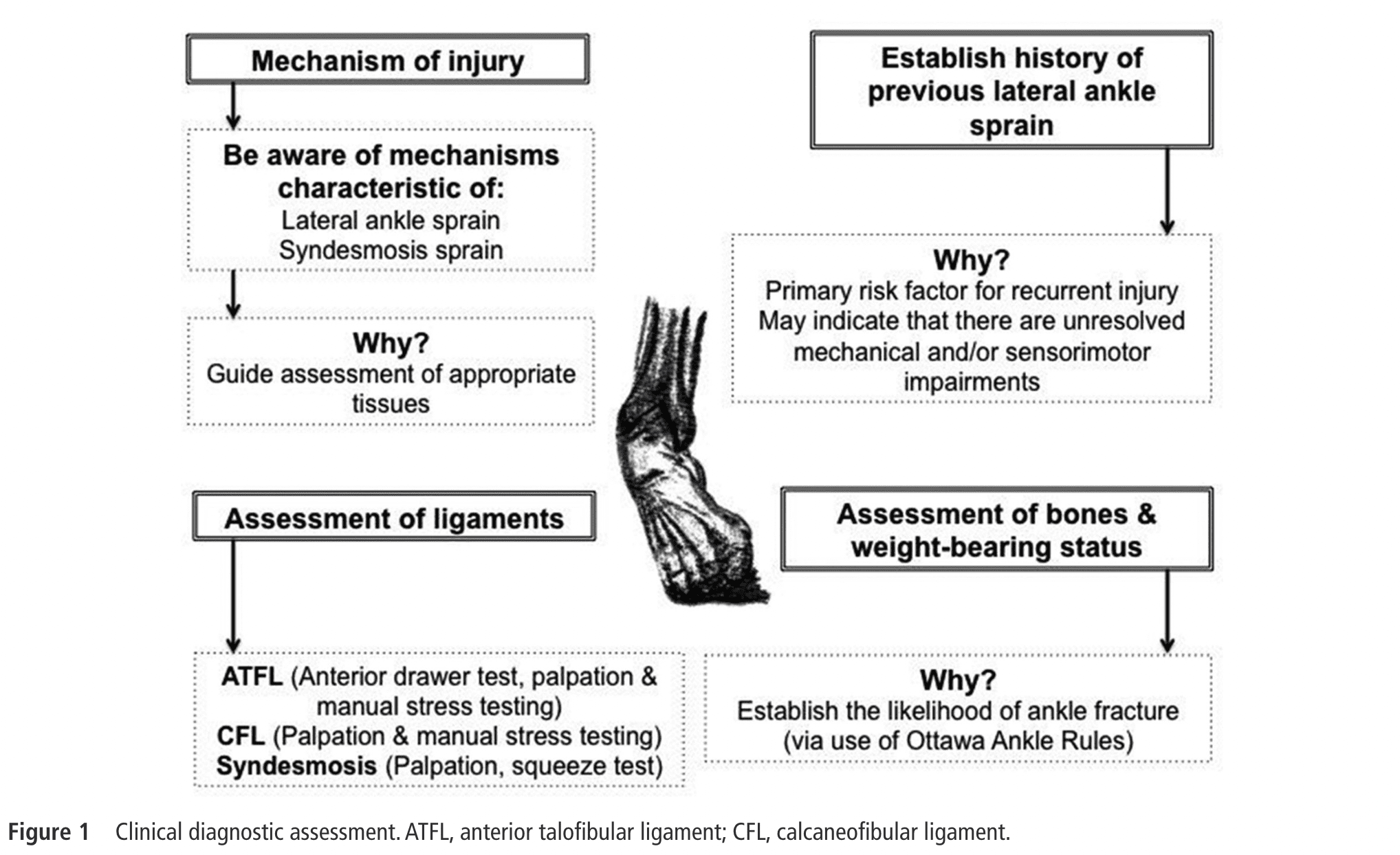
Evaluate the severity of the injury and determine the appropriate course of treatment. The examination should begin with a comprehensive history of the injury, including the mechanism of injury, any previous injuries or surgeries, and any associated symptoms such as pain, swelling, or instability (Delahunt et al 2018).
A history of previous sprains is associated with mechanical and sensorimotor impairments and heightens the risk of reinjury (Delahunt et al 2019).
Examination
Next, a physical examination should be performed to assess the extent of the injury. This should include an assessment of ankle range of motion, strength, and stability. Specific tests should also be performed to evaluate the integrity of the ligaments, such as the anterior drawer test, the talar tilt test, and the external rotation stress test. These are described below.
Anterior drawer test
The anterior talofibular ligament is most often injured. Replication of the known pain when palpating or stressing the ligament with passive plantar flexion and inversion is indicative of injury. The anterior drawer test to assess for complete disruption are best performed after 4 to 6 days. A positive test results in a sulcus sign (van Dijk et al 1996).
Talar tilt test
This test can stress the anterior talofibular ligament and/or calcaneofibular ligament, depending on the execution.
External rotation stress test
This test will stress the syndesmosis. It is important to rule out or rule in concomitant or isolated syndesmotic injuries with ankle sprains.
Calcaneofibular Ligament
Assessing the calcaneofibular ligament is possible with palpation or stressing the ligament in passive dorsiflexion with inversion. Do note that the ligament is crossed by the peroneal tendons and sheaths, making it directly palpable for approximately 1 cm. The stress tests should replicate the known pain to be positive.
Ottawa Ankle Rules
To exclude possible fractures we can trust the Ottawa ankle rules. An inability to weight-bear four steps after injury or pain on palpation on the posterior edge of the distal 6 cm of the medial or lateral malleolus should increase your suspicion of a possible fracture. If this is the case, an X-ray is warranted (Gomes et al 2022).
In addition to the physical examination, validated outcome measures can be used to assess the functional status of the ankle and monitor progress during rehabilitation. Examples of these measures include the Foot and Ankle Ability Measure (FAAM) and the Lower Extremity Functional Scale (LEFS).
A full list of things to evaluate can be seen in the table down below:
Other
Static postural balance, dynamic postural balance and gait should be assessed with for example the foot lift test and the star excursion balance test, respectively (Delahunt et al. 2019).
Imaging
Depending on the severity of the injury, imaging studies such as X-rays, ultrasound, or MRI may be ordered to evaluate the extent of the damage and rule out other injuries such as fractures or dislocations. Overall, a thorough examination that considers both physical and functional aspects of the injury is important to accurately diagnose and manage acute lateral ankle sprains (Delahunt et al 2018).
High Ankle Sprain/Syndesmosis Injury
The prevalence of ankle joint syndesmosis ligament injury, with or without the involvement of the lateral ligaments, has been reported to be 20% (Roemer et al. 2014). Tenderness on palpation of the syndesmosis ligaments is the most sensitive test while the squeeze test is the most specific (Sman et al 2015). Both being positive results in a high probability of injury to the syndesmosis ligaments.
Palpation Syndesmosis Ligaments
Squeeze test
External rotation stress test
LEVEL UP YOUR ROTATOR CUFF DISORDER KNOWLEDGE – FOR FREE!

Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
Quantifying pain during rehab is endorsed to guide the progression of exercise-based rehab. Other variables to consider are swelling and ROM, measured with the figure-of-eight method and the weight-bearing lunge test, respectively.
To learn about the figure-of-eight method, watch this video:
Rest, ice, compression, elevation (RICE)
The efficacy of ice and compression in reducing injury-associated symptoms following acute LAS is not well supported by trials. While cryotherapy has been investigated in 33 randomized controlled trials with a total of 2337 participants, the limited available evidence suggests that its efficacy for reducing acute LAS symptoms is unclear. The efficacy of RICE alone, cryotherapy alone, or compression therapy alone in improving pain, swelling, or patient function for acute LAS is not supported by evidence. Therefore, physiotherapy practitioners should carefully evaluate the use of cryotherapy and consider alternative treatment methods for individuals with acute LAS. (Vuurberg et al. 2018).
Medication
Patients with acute LAS may use NSAIDs to alleviate pain and swelling, but caution should be exercised as their usage is associated with complications and may inhibit or delay the natural healing process (Vuurberg et al. 2018).
Resistance training
Individuals with chronic ankle joint instability have deficits in ankle joint strength so assessing this via handheld dynamometers is recommended (Delahunt et al. 2019). Evidence suggests that hip strength is decreased as well in individuals with chronic ankle instability, targeting this might be something to consider (McCann et al. 2017).
Exercise
Physical therapists are recommended to consider initiating exercise therapy programs early after an acute LAS injury, as these programs have been found to reduce the prevalence of recurrent injuries and functional ankle instability, as well as lead to faster recovery and improved outcomes. For patients with severe ankle sprains, supervised physiotherapy may be more effective than a home exercise program, improving ankle strength and proprioception and enabling faster return to work and sports. However, it is important to note that some studies have contradicted these findings, showing no effect from adding supervised exercise therapy to conventional treatment alone or no improvement in postural balance after exercise therapy. Therefore, exercise therapy programs should be carefully individualized based on patients’ needs, with the level of supervision and guidance determined accordingly (Vuurberg et al. 2018).
Furthermore, assessing the individual’s preinjury participation level is paramount for the specificity of your exercise program (Delahunt et al. 2019).
Recent studies have shown that most rehabilitation exercises prescribed in current RCTs are generic, simplistic, and do not fully address the pathomechanics of non-contact lateral ankle sprains, which may limit the effectiveness of LAS rehabilitation. Exercise intervention should incorporate joint position sense training, multi-directional movements, flight phases, and single limb landings in a progressive manner (Wagemans et al. 2022).
Manual therapy
Manual therapy in the form of joint mobilizations is best combined with an exercise program. Mobilizations and exercise appear to be superior to home exercise alone (Cleland et al. 2013). They appear to increase dorsiflexion ROM in the short-term and decrease pain (Loudon et al. 2013).
Surgery
Surgery is rarely needed unless additional structural integrities are damaged such as the fibula. ‘Simple’ acute sprains are managed conservatively, eventual chronic instability might require surgery (Al-Mohrej et al. 2016).
References
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
ORTHOPEDIC PHYSIOTHERAPY OF THE UPPER AND LOWER EXTREMITIES