ACL Tear
Body Chart

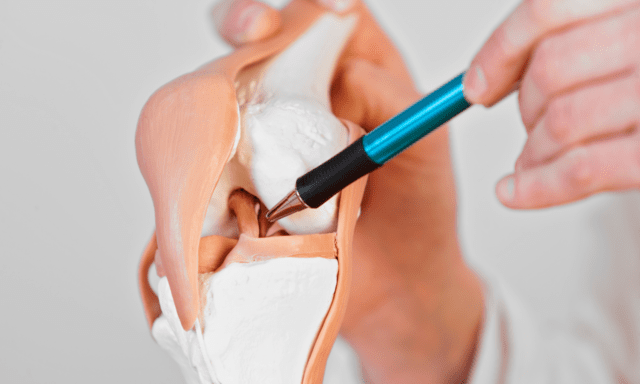
Ventral and dorsal aspects of the knee
Background Information
Patient Profile
- ~250.000 annual incidence
- Women 4-6x higher risk for rupture in “high risk” sports
Pathophysiology
Mechanism of injury
Abrupt deceleration, hyperextension, and rotation on fixated foot; Audible rupture
Source
- Atrophy or weakness; plyometric deficits
- Capsule/ligament damage or degeneration
- Knee valgus; Hip adduction & internal rotation; external rotation of tibia
Grades
- Grade I: Mild irritation, no rupture
- Grade II: Overstretch with partial rupture
- Grade III: Complete rupture
Acute: Pain- and tissue healing mechanisms align
- Inflammation phase: Dominant inflammatory nociceptive: signs of inflammation, night pain, pulsating, immobilization leads to stiffness, sometimes increases with rest
- Proliferation phase: Dominant mechanical nociceptive: clear on/off behavior, load dependent pain, local, decreases with rest
Chronic: Pain- and tissue healing mechanisms do not align
- Dominant mechanical nociceptive: clear on/off behavior, load dependent pain, local, decreases with rest
Course
Conservative treatment with optional surgery resulted in 50% of patients not needing surgery
Surgical: Rerupture rate in contact sports (25-30%)8, 6-12 months until RTP
History & Physical Examination
History
History of knee trauma; knee exposed to high loads in work, sport, ADLRecent trauma: heard “popping” “snapping”, immediate swelling
- “Giving way” a/p and in rotation is the main criteria
- Feeling of instability in rotatory or a/p direction
- Acute: Marked hematoma and limited ROM; local pain, stinging, deep
- Chronic: Feeling of instability; “giving way” despite healed tissues
Physical Examination
Inspection
Acute: Signs of inflammation; possible hemarthrosis; intraarticular swelling; protective posture
Chronic: Quadriceps/gastrocnemius atrophy, barely any swelling
Functional Testing
Acute: not possible due to symptoms
Chronic: Deep squat, climbing stairs, cutting motion, “giving way” rather described than demonstrated
Active Examination
Acute: limited ROM in Flex/Ext/Rot and pain upon small load
Chronic: end of range limitation in Flex/Ext/Rot; high loads in combination with these movements is painful; balance problems: single leg stance, step-up
Special Testing
Passive Examination
Acute: PROM limited, swelling masks structural instability
Chronic: End or range ROM limited, Structural instability apparent
Differential Diagnosis
- Subchondral injury
- Damaged cartilage
- Gonarthrosis
- Avulsion fracture biceps femoris
- Tibial plateau fracture
- Unhappy triad
- Pes anserinus irritation
- Patella luxation
- PFPS
- Quadriceps tendon rupture
- Patella tendon rupture
- Osgood Schlatter
Treatment
Strategy
Conservative: coper, isolated injury, >45 years old, linear sports
Surgical: non-coper, multidirectional injury, <45 years old, high-risk sports
Interventions
Post-OP
Reach milestones of each rehabilitation phase before progressing. Adapt to tissue healing phases
Conservative
Identify deficits in strength, neuromuscular control, passive structures
Principles
Concentric before eccentric, slow to fast, low load + high rep to high load + low rep, two-legged to one-legged, pay attention to sport specific demands
References
- Adams, D., Logerstedt, D. S., Hunter-Giordano, A., Axe, M. J., Snyder-Mackler, L. (2012). Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther, 42(7), 601-614. doi:10.2519/jospt.2012.3871
- Boden, B. P., Sheehan, F. T., Torg, J. S., & Hewett, T. E. (2010). Noncontact anterior cruciate ligament injuries: mechanisms and risk factors. J Am Acad Orthop Surg, 18(9), 520-527.
- Frobell, R. B., Roos, E. M., Roos, H. P., Ranstam, J., Lohmander, L. S. (2010). A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med, 363(4), 331-342. doi: 10.1056/NEJMoa0907797
- Hewett, T. E., Di Stasi, S. L., Myer, G. D. (2013). Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med, 41(1), 216-224. doi: 10.1177/0363546512459638
- Howell, R., Kumar, N. S., Patel, N., & Tom, J. (2014). Degenerative meniscus: Pathogenesis, diagnosis, and treatment options. World J Orthop, 5(5), 597-602. doi: 10.5312/wjo.v5.i5.597
- Lange, A. K., Fiatarone Singh, M. A., Smith, R. M., Foroughi, N., Baker, M. K., Shnier, R., Vanwanseele, B. (2007). Degenerative meniscus tears and mobility impairment in women with knee osteoarthritis. Osteoarthritis Cartilage, 15(6), 701-708. doi:10.1016/j.joca.2006.11.004
- Mandelbaum, B. R., Silvers, H. J., Watanabe, D. S., Knarr, J. F., Thomas, S. D., Griffin, L. Y., Garrett, W. (2005). Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med, 33(7), 1003-1010. doi: 10.1177/0363546504272261
- Paterno, M. V., Schmitt, L. C., Ford, K. R., Rauh, M. J., Myer, G. D., Huang, B., Hewett, T. E. (2010). Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med, 38(10), 1968-1978. doi: 10.1177/0363546510376053
- Powers, C. M. (2010). The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther, 40(2), 42-51. doi: 10.2519/jospt.2010.3337
- Shea, K. G., Carey, J. L., Richmond, J., Sandmeier, R., Pitts, R. T., Polousky, J. D., Sevarino, K. (2015). The american academy of orthopaedic surgeons evidence-based guideline on management of anterior cruciate ligament injuries. J Bone Joint Surg Am, 97(8), 672-674.
- Snyder-Mackler, L., Risberg, M. A. (2011). Who needs ACL surgery? An open question. J Orthop Sports Phys Ther, 41(10), 706-707. doi: 10.2519/jospt.2011.0108
- Zazulak, B. T., Hewett, T. E., Reeves, N. P., Goldberg, B., & Cholewicki, J. (2007). Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med, 35(7), 1123-1130. doi: 10.1177/0363546507301585


