HSR for Lateral Elbow Tendinopathy

Introduction
Various treatments exist for lateral elbow tendinopathy, also called lateral epicondylalgia. It is difficult for the clinician to inform people about the best available treatment, both from a pain and functional improvement perspective and from a structural integrity perspective, as there is uncertainty about the superior treatment combinations. Among the most encountered treatment options in physiotherapy practice are heavy slow resistance (HSR) training and tendon dry needling. These options are frequently supplemented by corticosteroid injections.
While studies on isolated progressive resistance training, such as HSR, have demonstrated superior short- and long-term effects in patellar and Achilles tendinopathy, the results for lateral elbow tendinopathy were conflicting. Likewise, it remains unknown if a corticosteroid injection or dry needling combined with an HSR program is superior to an HSR program alone for lateral elbow tendinopathy. Therefore, the current study was set up.
Methods
This study addresses a critical question in the management of lateral elbow tendinopathy: whether adding corticosteroid injections (CSI) or tendon needling (TN) to a heavy slow resistance (HSR) training program offers superior outcomes compared to HSR alone.
A 3-arm randomized, double-blinded, placebo-controlled trial was conducted in Denmark to investigate the effects of heavy slow resistance (HSR) training combined with either a corticosteroid injection (CSI), tendon dry needling (TN), or placebo needling (PN) for chronic unilateral lateral elbow tendinopathy.
The study included adults aged 18 to 70 years who had lateral elbow tendinopathy symptoms for at least three months. Key diagnostic criteria included clinical symptoms of lateral elbow pain and/or forearm pain and tenderness on palpation of the lateral humeral epicondyle. These clinical symptoms had to be reproduced in at least two of three specific tests:
- Cozen test
- Maudsley test
- forearm supination test
Furthermore, the Disabilities of the Arm, Shoulder and Hand (DASH) score was completed at baseline. The requirement for inclusion was a DASH score greater than 30 points. Besides the clinical requirements, ultrasonographic evidence of increased tendon thickness, hypoechoic signals, or pathological power Doppler activity within the common extensor tendon origin was necessary before someone was eligible for inclusion.
Patients with previous fractures, osteoarthritis, bilateral symptoms, systemic arthritis, diabetes, or those who had received a CSI or dry needling within the prior three months were excluded.
The primary outcome was the DASH score, which assesses upper extremity function and symptoms, at 52 weeks (1 year). This questionnaire contains 30 questions, addressing function and symptoms over the past week, rated from 1 to 5. The total score ranges from 0 (no disability) to 100 (severe disability).
- A DASH score below 15 points indicates no problem, while 16-40 points suggest a problem, but the individual is still able to work. Scores above 40 points signify an inability to work and significant functional difficulties. It has been proposed that a DASH score under 30 points means patients no longer consider their upper extremity disorder a problem. A score between 10-29 points is a benchmark for returning to work, where patients are aware of limitations but don’t view them as problematic. The minimal clinically important difference for the DASH score is 12 points.
Secondary outcomes included the shortened QuickDASH score, pain intensity measured by an 11-point Numerical Rating Scale (NRS), pain-free grip strength (measured with a digital hand dynamometer), and hypervascularization (assessed by power Doppler ultrasonography). These were measured at baseline, 12, 26, and 52 weeks.
Interventions
Every included participant received an “injection”, which was followed by a 12-week HSR protocol.
As there were 3 groups, three different “injections” were used
- Corticosteroid Injection (CSI): 1 mL of Depo-Medrol (40 mg/mL) and 1 mL of lidocaine (10 mg/mL) injected beneath the affected tendon, guided by ultrasound.
- Tendon Needling (TN): The needle was inserted through the affected tendon at 2-3 sites, combined with an injection of 1 mL of 0.9% isotonic saline, guided by ultrasound.
- Placebo Needling (PN): 1 mL of 0.9% isotonic saline injected just below the skin, ensuring no contact with the tendon, guided by ultrasound.
Important Note: For all injections, the syringe was covered, and the ultrasound screen was hidden from the participant to maintain blinding.
Then every participant started the Heavy Slow Resistance (HSR) training program after receiving their injection, with a mandatory two-day rest period post-injection. The program was performed at home three times per week, with a minimum of one day of rest between sessions.
Exercises: The program consisted of three different exercises targeting extension, flexion, and supination/pronation of the hand, adapted from principles used for patellar and Achilles tendinopathy. The training load was progressively increased using elastic bands with varying resistance:
- Week 1: 3 sets of the 15 repetition maximum (RM) for each exercise.
- Weeks 2-3: 3 sets of 12 RM.
- Weeks 4-5: 3 sets of 10 RM.
- Weeks 6-8: 3 sets of 8 RM.
- After Week 8: 3 sets of 6 RM.
All of the exercises were performed slowly, with three to four seconds in each direction (concentric and eccentric phases). Two minutes of rest were provided between each set.
Patients were instructed that pain up to 5 out of 10 on the NRS was acceptable during and after HSR, if it subsided shortly after exercise or if the load was adjusted. They were also advised to avoid other activities or exercises that increased pain above this level. A training diary was used to track progression. A control visit with a physical therapist at week 4 ensured correct exercise performance and progression.
Results
A total sample of 58 participants was analyzed, with 21 participants in the CSI group, 17 in the dry needling group, and 20 in the placebo needling group. At baseline, the groups were equal, according to the authors, with regard to demographics, symptom duration, activity levels, and primary and secondary outcome measures.
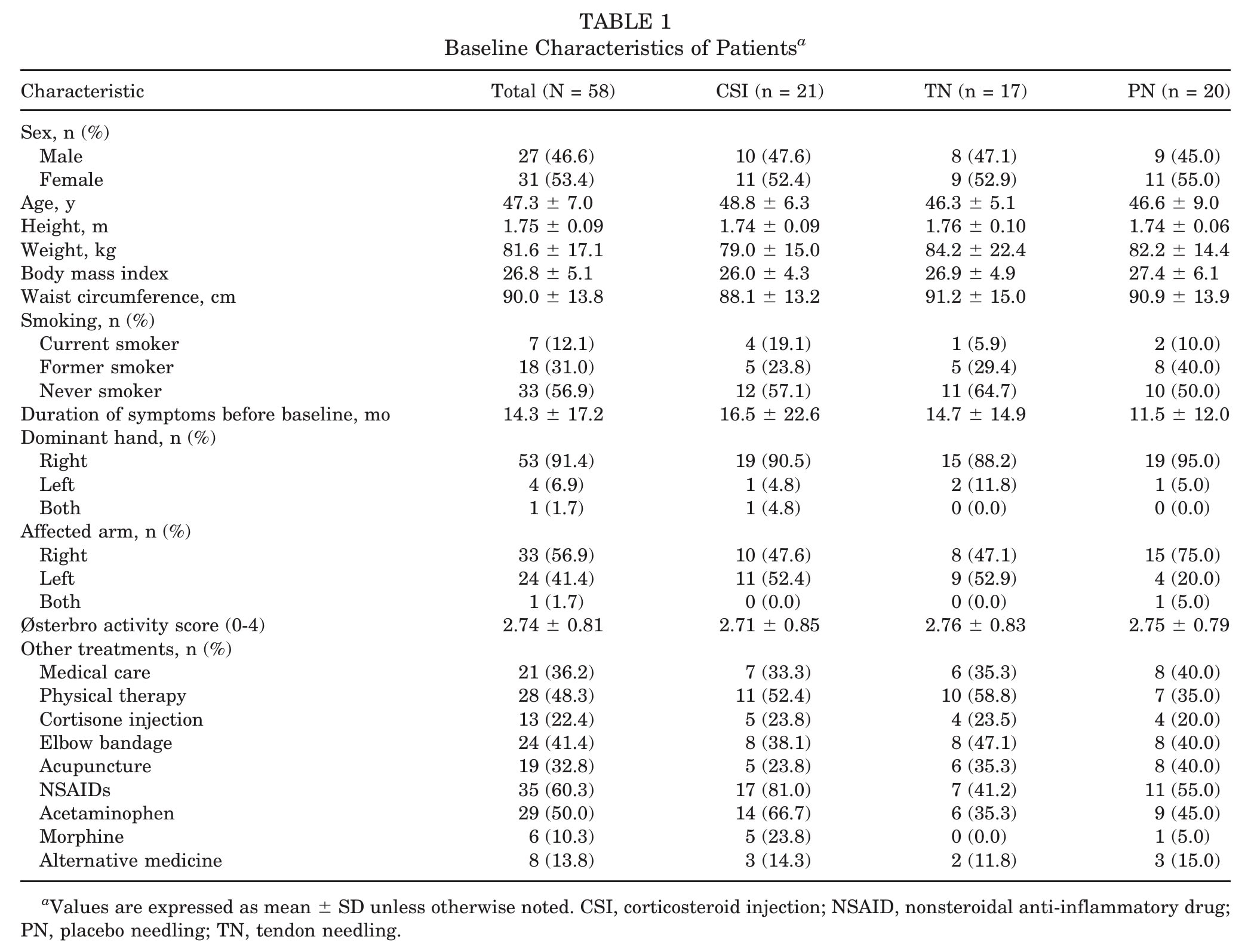
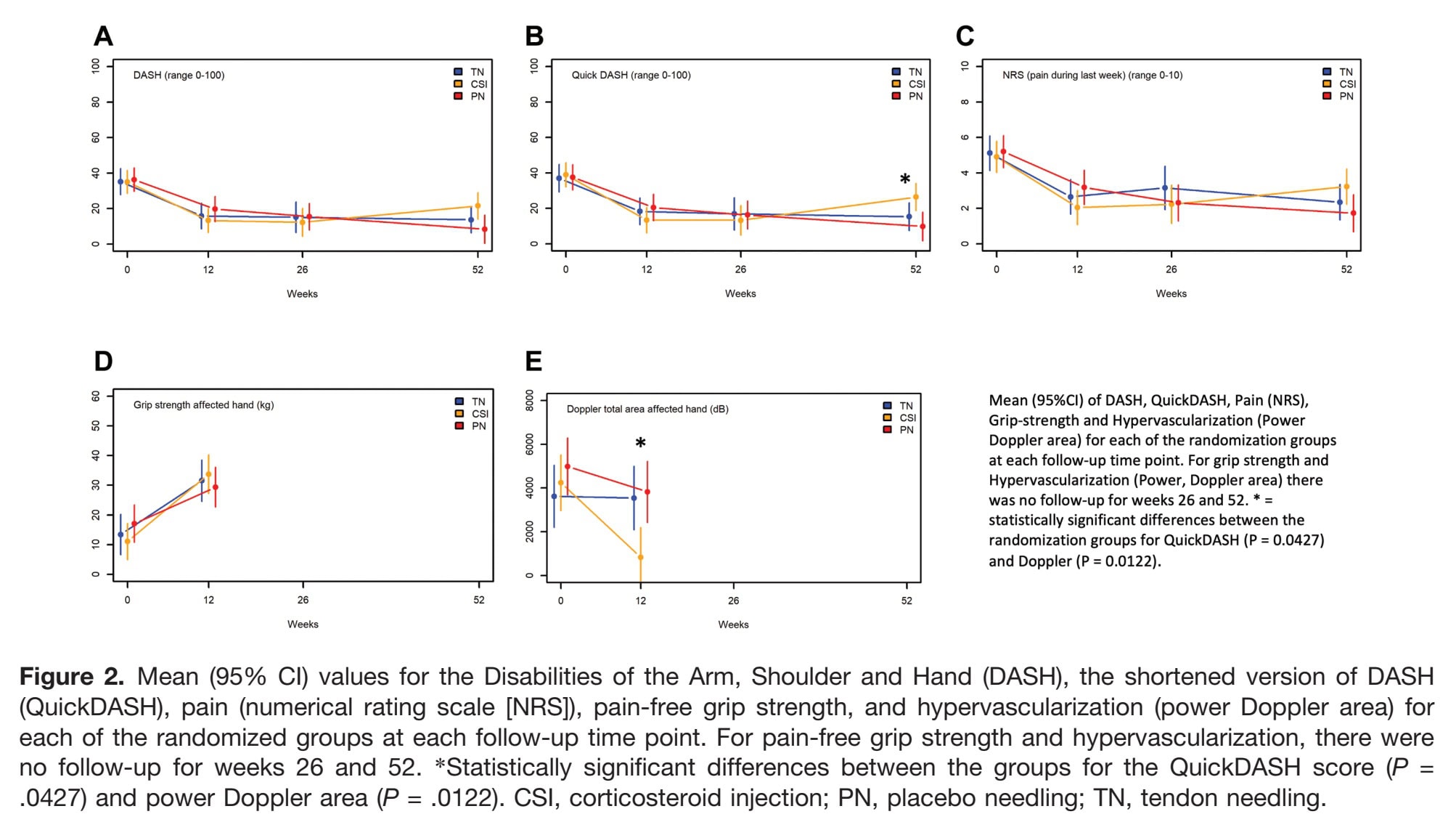
Within-group comparisons showed that all groups improved across all patient-reported outcomes (DASH, QuickDASH, NRS) after 12, 26, and 52 weeks. Pain-free grip strength improved from baseline to 12 weeks for all groups, and hypervascularization decreased markedly in the CSI group but not in the PN and TN groups.
The between-group effects revealed no significant overall differences in DASH improvements at 12 or 26 weeks. At 52 weeks, the overall comparison still did not reach statistical significance (p=.0581), but pairwise analyses (Table 2) showed that the CSI group had significantly higher (worse) DASH scores compared to the PN group (p=.0176).
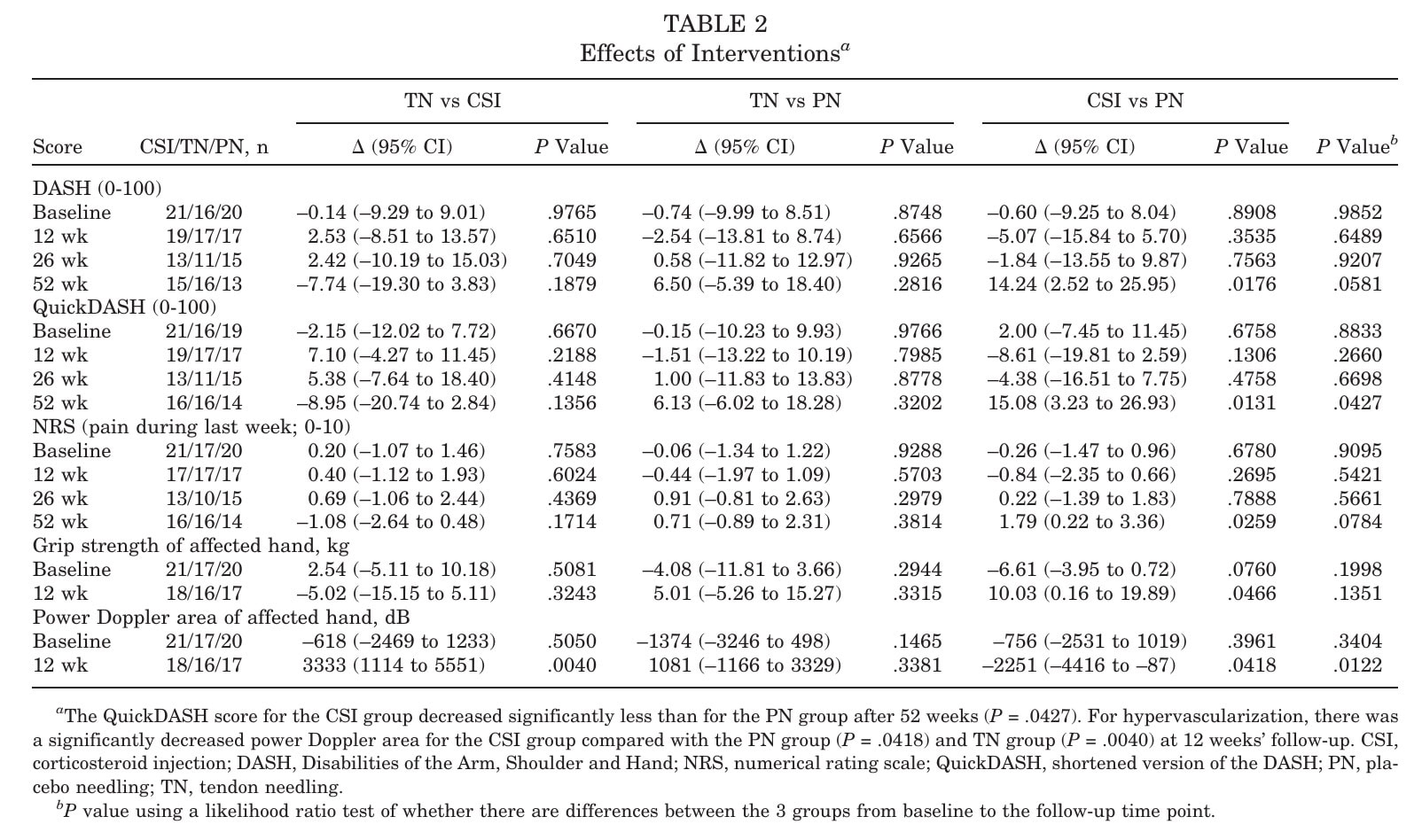
Secondary outcomes
The QuickDASH at 52 weeks demonstrated the same pattern as the DASH, with significantly worse scores in the CSI group compared to PN (p=.0427).
For pain (NRS), no differences were observed between groups at 12 or 26 weeks. At 52 weeks, the CSI group reported more pain than the PN group (pairwise p=.0259), though the overall test across all three groups was not significant. This suggests that the long-term effect of CSI may be detrimental compared to HSR plus placebo.
Short-term benefits were observed in the CSI group at 12 weeks, with significantly higher grip strength compared to PN (p=.0466), alongside a sharp reduction in hypervascularization. However, these structural and strength changes did not translate into sustained clinical benefit.
The authors also analyzed the area under the curve (AUC) for DASH across all time points (baseline, 12, 26, 52 weeks) and found no overall differences between groups. This explains why they emphasize the general similarity across groups, despite the 52-week pairwise effects. Importantly, the worsening seen in the CSI group was not only statistically significant but also clinically meaningful (≥MCID thresholds).
In summary, all participants improved with HSR for lateral elbow tendinopathy regardless of add-on intervention. CSI, however, was associated with worse self-reported function and pain in the long term.
Questions and thoughts
Should we now prescribe HSR for lateral elbow tendinopathy for every patient? This trial strongly supports HSR as a first-line strategy: it produced consistent, clinically meaningful improvements across outcomes. Yet, patients in acute pain may still request a “quick fix.” While corticosteroid injections can reduce hypervascularization and provide short-term changes, this study demonstrated that CSI worsened pain and function at 52 weeks. Patients should be informed of this risk when considering CSI.
All participants improved within groups, reinforcing the value of HSR for lateral elbow tendinopathy. Still, the study did not correct for multiple comparisons, a limitation acknowledged by the authors. This means that some statistically “positive” pairwise findings (e.g., grip strength at 12 weeks) should be interpreted with caution.
Another point is hypervascularization: only the CSI group showed clear reduction, but this was not mirrored in functional outcomes. This highlights a broader issue — structural imaging changes do not necessarily align with patient-reported outcomes, and functionality may matter more than pathology resolution.
Compliance with the HSR program was excellent: participants completed 83% of sessions (269/324 on average). That is remarkable for a heavy-load program, suggesting that the physiotherapists’ careful instruction and monitoring were crucial. By contrast, a feasibility study by Sveinall et al. (2024) reported only 32% compliance in unsupervised HSR, due to pain aggravation. This underscores that HSR can work well, but only if patients are supported and educated.
Talk nerdy to me
Randomization was stratified by sex and baseline DASH score. Participants, statisticians, research assistants, and physiotherapists were blinded; only the trial physicians knew allocations. Still, blinding was not perfect: 52% of CSI and 58% of PN participants guessed correctly, higher than the 33% expected by chance. This may have biased patient-reported outcomes.
Although the groups were reported as equal at baseline, pain medication use was uneven. For example, morphine use was 23.8% in the CSI group but only 5% in PN. NSAID and acetaminophen use was also higher in CSI. This imbalance threatens internal validity: being on morphine could alter how participants perceived or reported pain, potentially masking or inflating intervention effects. While randomization aims to balance such factors, chance imbalances in small trials can confound results.
I noted some apparent contradictions between overall and pairwise comparisons. To clarify:
- Overall tests (like ANOVA or mixed models across all groups) ask whether all three groups differ together. Here, no overall differences were found at 52 weeks for DASH, QuickDASH, or NRS.
- Pairwise tests look at specific contrasts (CSI vs PN, CSI vs TN, TN vs PN). These did reveal significant differences, e.g., CSI vs PN at 52 weeks.
- This discrepancy happens because overall tests have less power to detect isolated group differences, and because multiple pairwise tests inflate the risk of type I error. The authors did not adjust for multiple comparisons, which further complicates interpretation.
The reporting issue is that the text sometimes emphasizes “no differences” while the tables show significant pairwise p-values (e.g., CSI vs PN grip strength at 12 weeks, p=.0466). Without clarifying whether adjustments were made, this can be misleading. According to CONSORT, all significant results should be transparently reported. The authors acknowledged the risk of inflated type I error but left it to the reader to adjust — not ideal practice.
Finally, the authors themselves questioned whether DASH is sensitive enough for this condition. They noted that the Patient-Rated Tennis Elbow Evaluation would have been a more specific tool, but it lacked a validated Danish version. This limitation may have blunted their ability to detect subtle but real between-group differences.
Take-home messages
For individuals with lateral elbow tendinopathy, a home-based Heavy Slow Resistance (HSR) training program using simple elastic band exercises appears to be effective in improving symptoms and function in both the short and long term. Adding corticosteroid injections (CSI) or tendon dry needling (TN) to this HSR program did not enhance its benefits and, in the case of CSIs, seemed to negatively impact patient-reported outcomes over the long term. Therefore, focusing on HSR training along with good instructions on pain levels and progression may be the most beneficial approach.
Reference
Watch two 100% Free Webinars on Shoulder Pain and Ulna-Side Wrist Pain
Improve your Clinical Reasoning for Exercise Prescription in the Active Person with Shoulder pain with Andrew Cuff and Navigate Clinical Diagnosis & Management featuring a Case Study of Golfer with Thomas Mitchell