Cách các chuyên gia vật lý trị liệu trấn an bệnh nhân hiệu quả trong các buổi tư vấn về đau lưng. Một nghiên cứu định tính.

Giới thiệu
Reassurance remains one of the most potent yet challenging interventions in back pain management. As highlighted in a recent Physiotutors review, patients’ expectations about treatment—particularly exercise—significantly influence their pain and functional outcomes, both short- and long-term. Emerging evidence suggests that therapeutic education and collaborative care can reshape unhelpful beliefs.
Many clinicians still struggle to deliver reassurance effectively. Time pressures, competing priorities, and communication gaps often leave patients’ core concerns unaddressed, eroding therapeutic trust.
Research underscores the value of combining cognitive reassurance (clear, evidence- based explanations) with affective reassurance (empathy and rapport-building) to empower patients and promote self-management. Yet, the question remains: How can clinicians refine their approach to reassurance in everyday practice?
This qualitative study examines the subtleties of effective reassurance in physiotherapy, providing actionable strategies to enhance therapeutic trust and patient recovery.
Phương pháp
This study analyzed video recordings of 20 initial physiotherapy consultations (10 therapists, 20 patients) collected in 2016 as part of a larger investigation into cognitive functional therapy (CFT) training. Twelve therapists were purposively selected to represent diversity in gender, age, clinical experience (4-14+ years), and had received a post graduate biopsychosocial training (0-12 days).
Patients (ages 26-67) with chronic nonspecific LBP (>3 months) were recruited from two UK physiotherapy departments. Patients completed the Ørebro Musculoskeletal Pain Screening Questionnaire (ØMPSQ), Roland Morris Disability Questionnaire (RMDQ), STarTBack Screening Tool, and a 0-10 Pain Numerical Rating Scale (NRS). Consultations lasted 35-60 minutes and were video recorded with a researcher present to manage equipment. Seven initially recruited patients were excluded (1 declined recording, 4 resolved symptoms, 2 no-shows), leaving 20 participants (11 women, 9 men) for analysis.
This study employed conversation analysis (CA) as a qualitative framework to investigate how effective reassurance in physiotherapy is co-constructed during clinical consultations.
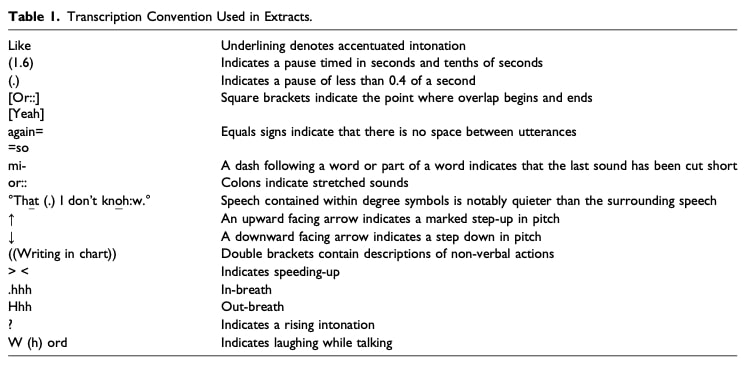
The video-recorded consultations were first transcribed verbatim by professional transcribers to establish a baseline record of the interactions. These transcripts were then refined using detailed Jeffersonian notation, which preserves the fine-grained features of speech—including pauses, intonation, overlaps, and prosody—as well as relevant non-verbal behaviors (e.g., gaze, gestures, posture) annotated in context. This level of detail was essential for understanding not just what was said, but how it was delivered and received.
Guided by CA principles, the analysis focused on core dimensions of interaction:
- Turn-taking – How participants organized their speech transitions, includinginterruptions, smooth handovers, or competitive overlaps, revealing powerdynamics and engagement.
- Sequence organization – How each utterance led to the next, particularly howreassurance was initiated, developed, and responded to across multiple turns.
- Turn design – The phrasing, framing, and pragmatic strategies (e.g., hedging, emphatic statements) used to deliver reassurance.
- Lexical choice – The specific word selections (e.g., “normal” vs. “common”) and their implications for shaping patient perceptions.
- Interactional asymmetry – How institutional roles (clinician vs. patient) influenced participation, such as who controlled topic shifts or question-answer patterns.
- Non-verbal coordination – The alignment (or misalignment) between speech and body language, such as nodding while affirming a patient’s concern.
- Consultation structure – The broader arc of the encounter, from openings (e.g., rapport-building) to closings (e.g., summarizing next steps), and where reassurance strategically appeared.
Two researchers independently analyzed conversations to pinpoint reassurance moments, then compared findings to minimize bias. Their approach carefully balanced natural observation of interaction patterns with awareness of how clinical backgrounds might shape interpretations. Through this process, the analysis identified both overt and nuanced factors that determine whether effective reassurance in physiotherapy succeeds or fails in clinical dialogues.
Kết quả
Findings revealed a spectrum of effective reassurance in physiotherapy practices during back pain consultations, ranging from collaborative, patient-centered approaches to less successful, therapist-dominated interactions.
Physiotherapist reassurance not targeted to patient’s concerns
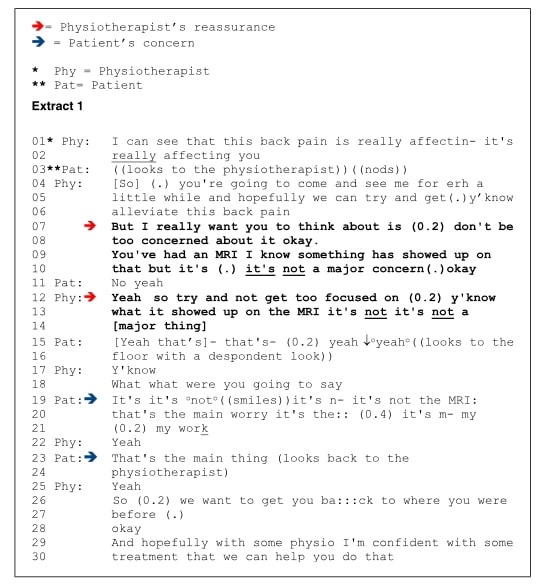
Research has identified that physiotherapists may presuppose patients’ primary concerns, often minimizing their reported findings. Verbatim examples include: “It’s not… it’s not a [major thing]” (physiotherapist discussing back MRI results). Analysis of three other cases revealed this consistent pattern of downplaying imaging findings. Given that imaging results frequently don’t correlate with pain or functional limitations, these cases suggest such findings may not be patients’ main concern—yet physiotherapists frequently provide unsolicited education about them.
The studies also found that some practitioners struggle to create space for patients to voice their beliefs and concerns. When patients attempt to redirect conversations— through verbal cues like hesitant “[Yeah that’s]- that’s,” or nonverbal signals like the despondent “o↓yeaho” while looking downward—therapists may miss these opportunities. In one case, when a patient clarified that returning to work—not scan results—was his primary worry, the physiotherapist responded with generic reassurance: “I’m confident… we can help you do that,” rather than exploring his specific concerns.
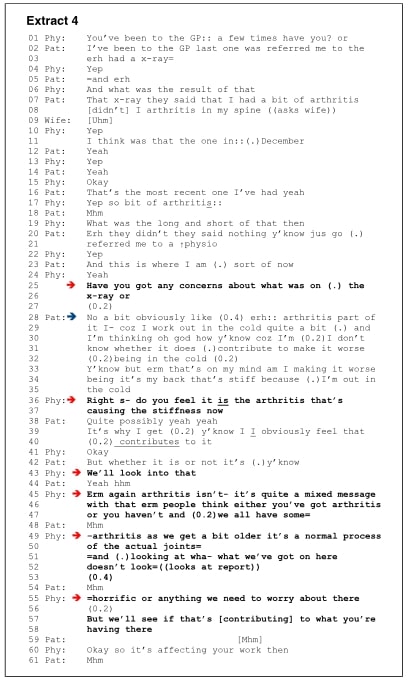
Additionally, therapists sometimes deliver mixed messages. One clinician initially engaged with a patient’s arthritis concerns (“We’ll look into that”), but later contradicted this by calling spinal arthritis universal (“we all have some”) and “a normal process.” Language choices also mattered—phrases like “doesn’t look horrific or anything we need to worry about” introduced unnecessary alarm through terms like “horrific.”
Disconfirming patient’s fears via behavioral experiment
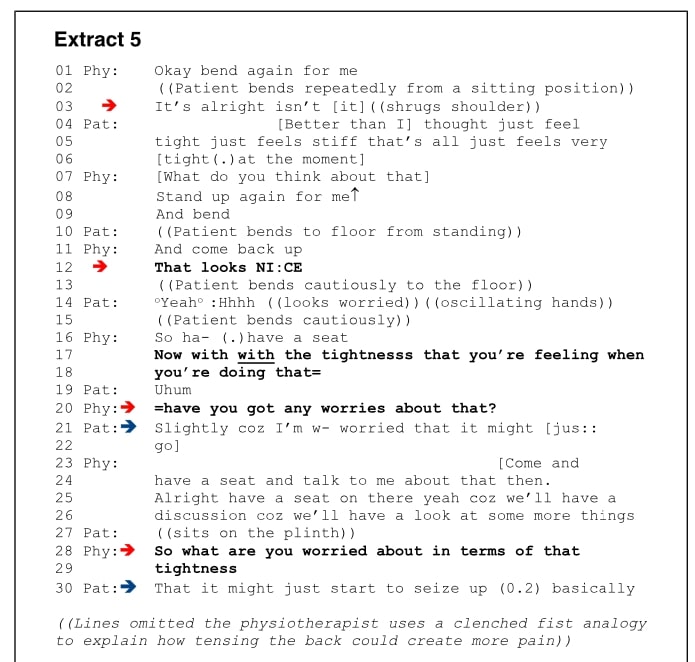
The clinical interaction in Extract 5 demonstrates an effective approach to managing a patient’s fear of bending forward (“going to hurt my back”). The physiotherapist began by exploring the movement gradually, first from a seated position while providing positive feedback: “It’s alright, isn’t it?” When progressing to the patient’s specifically feared movement—standing bending, which he associated with excessive “distance”— the therapist astutely observed the patient’s anxious nonverbal cues and created space for discussion by asking, “Have you got any worries about that?”
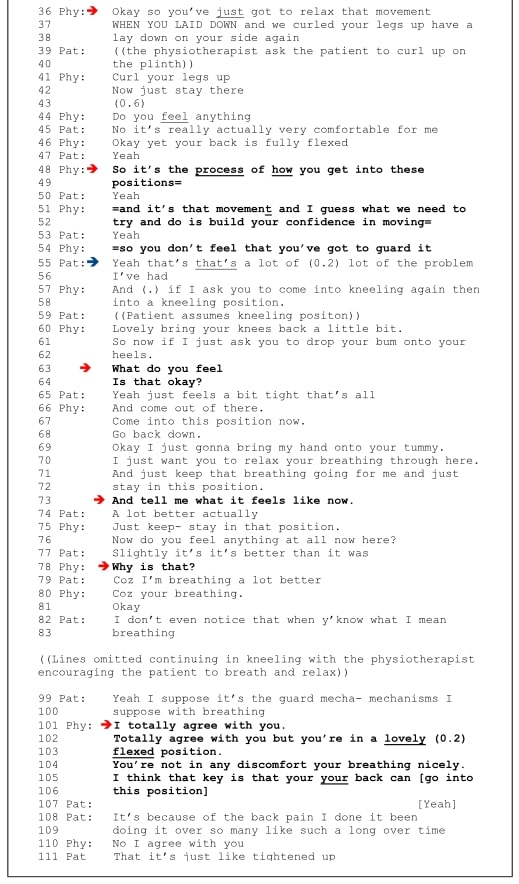
The session then transitioned to belief modification through physical demonstration. By guiding the patient into an unloaded side-lying position with knees flexed to chest—a fully flexed spinal position the patient normally feared—and asking “Do you feel anything?,” the therapist created a powerful experiential contradiction when the patient responded, “No, it’s really actually very comfortable.” This concrete demonstration that flexion could be pain-free led to a key reframing moment, where the therapist suggested, “the problem is not bending per se but how you bend: ‘it’s the process of how you get into these positions.'” The patient’s meaningful agreement—”Yeah, that’s… that’s a lot of the problem I’ve had”—confirmed this shift in understanding.
The intervention culminated in practical application, incorporating breathing techniques during bending movements to reduce protective guarding. The patient’s immediate feedback—”A lot better actually” and “it’s better than it was”—demonstrated tangible progress, which the therapist reinforced through reflective validation (“I totally agree with you”) regarding the guarding mechanisms.
This case exemplifies how combining gradual exposure, physical demonstration of safety, cognitive reframing, and immediate positive reinforcement provides effective reassurance in physiotherapy by addressing movement-related fears. It underscores that reassurance in physiotherapy achieves its greatest impact when patients discover safety through their own movement experiences, supported by a therapist who both guides and validates their progress.
Question and thoughts
As researchers have identified, there appears to be a pattern where physiotherapists systematically discuss imaging findings even when patients have not raised them as a concern. This raises questions about the underlying assumption that patients are overly preoccupied with imaging results. Indeed, such presuppositions may lead to inadequate addressing of patients’ actual concerns, leaving them feeling misunderstood.
We must therefore examine this tendency to provide patients with generic education about imaging. Why does this occur? One possible explanation is the adoption of an expert posture, inducing a vertical relationship where the therapist assumes the role of knowledge-holder who must “educate” the patient. While likely unconscious, this dynamic may create an imbalance in the therapeutic relationship, positioning the patient as a passive recipient of knowledge rather than an active participant.
In contrast, a horizontal therapeutic relationship establishes equality between therapist and patient. This collaborative approach allows solutions to naturally arise from the patient’s lived experiences, with the therapist facilitating exploration and offering expert reframing when beneficial. Such a dynamic enhances the therapist’s ability to truly hear and accurately address patient concerns.
The final case study exemplifies effective reassurance in physiotherapy in practice, demonstrating this ideal therapeutic interaction. Through behavioral experiments like graded exposure to feared movements, patients develop crucial self-awareness and become active participants in their care. Evidence indicates that patients who physically engage with and comprehend their condition – supported by therapist reinforcement – experience more meaningful reassurance and likely better recovery outcomes.
Nói chuyện với tôi một cách ngớ ngẩn
This qualitative study adopts a non-statistical approach to examine reassurance techniques in physiotherapy. While it incorporates quantifiable scales such as the NPRS, ÖMPSQ, and RMDQ, these are not employed as primary outcome measures to infer clinical effectiveness. Instead, the study focuses on the subjective dimensions of therapeutic interactions, raising important questions about the nature of evidence when investigating inherently qualitative phenomena.
The Challenge of Studying Subjective Experience
Social research presents unique methodological challenges, as traditional statistical tools are often inadequate for capturing the nuances of patient perceptions and lived experiences. By definition, these elements resist quantification, necessitating alternative paradigms capable of exploring the construction of meaning within social interactions. Qualitative research, therefore, emerges as the most appropriate framework for addressing such questions.
Conversation Analysis and Ethnomethodological Foundations
The authors employ Conversation Analysis (CA), a methodology deeply influenced by phenomenological philosophy and ethnomethodology. Grounded in the phenomenological tradition, this paradigm recognizes that reality is subjectively constructed through individual and collective interpretation. Ethnomethodology, extends this perspective by examining how social order is practically achieved through everyday interactions.
Key analytical foci include:
- Turn-taking dynamics in dialogue
- Nonverbal communication (e.g., gestures, eye contact)
- Role negotiation between clinician and patient
In this context, therapeutic relationships are not predefined but are actively co- constructed through moment-to-moment interaction. For instance, a physiotherapist’s reassurance is not merely “delivered” but is shaped by reciprocal exchanges, where both parties contribute to defining what constitutes “progress” or “risk.”. This study provides empirical support for the ethnomethodological perspective, demonstrating that the most effective reassurance techniques emerge from collaborative therapeutic interactions. These interactions are characterized by: behavioral experimentation (gradual exposure to feared movement), egalitarian communication, and co-created treatment planning through mutual identification of the underlying factors contributing to or explaining the patient’s pain experience.
Scientific Rigor in Qualitative Inquiry
While the study’s subject matter is not quantifiable, its methodological rigor is upheld through standardized analytical protocols. CA provides a systematic framework for transcribing and interpreting interactions, ensuring reproducibility despite the inherently subjective nature of the data. By adhering to these principles, the study yields empirically grounded insights into the process of reassurance, complementing outcome- focused quantitative research.
Những thông điệp mang về nhà
This study redefines effective reassurance in physiotherapy as a co-constructed process, not a therapist-delivered intervention.
1. Listen Before Educating
- Patients’ primary concerns (e.g., returning to work) might differ from clinical focus areas (e.g., MRI findings). First explore their perspective before offering generic reassurance.
2. Replace Vertical with Horizontal Communication
- Avoid expert-led monologues about scans/biomechanics. Instead, use:
- Open-ended questions:”What worries you most?”
- Behavioral experiments: Graded exposure to feared movements to disprove fears experientially.
- Shared decision-making: Co-create treatment plans by aligning with patient priorities.
3. Language Matters
Avoid minimizing phrases (“It’s not horrific”) or mixed messages. Instead:
- Validate: “I hear this is limiting your daily life—let’s work on that.”
- Reframe: “Your scan shows normal changes; let’s focus on what your body can do.”
4. Use Non-Verbal Cues
- Patients’ hesitation, gestures, or tone often reveal unspoken fears. Pause and probe: “You seemed unsure when we tried that movement—can you tell me more?”
Bottom Line: Reassurance isn’t something you give—it’s something you build together through dialogue, experimentation, and shared goals.
Thẩm quyền giải quyết
CẢI THIỆN ĐÁNG KỂ KIẾN THỨC CỦA BẠN VỀ ĐAU LƯNG DƯỚI MIỄN PHÍ
5 bài học cực kỳ quan trọng mà bạn sẽ không được học ở trường đại học, giúp cải thiện việc chăm sóc bệnh nhân đau lưng dưới ngay lập tức mà không phải trả một xu nào