เอ็นอักเสบของกล้ามเนื้อหัวไหล่: แนวทางปฏิบัติทางคลินิกฉบับใหม่ ปี 2025

อาการปวดไหล่ที่เกี่ยวข้องกับกล้ามเนื้อหมุนหัวไหล่เป็นหนึ่งในอาการปวดกล้ามเนื้อและกระดูกที่พบบ่อยที่สุดที่พบในคลินิกปฐมภูมิและคลินิกกายภาพบำบัด อย่างไรก็ตาม การรักษาด้วยยาเกินความจำเป็น กลยุทธ์การประเมินที่ไม่สม่ำเสมอ และการพึ่งพาการตรวจด้วยภาพยังคงแพร่หลายอยู่
แนวทางการปฏิบัติทางคลินิกปี 2025 โดย Desmeules และคณะ ซึ่งตีพิมพ์ในวารสาร Journal of Orthopaedic & Sports Physical Therapy นำเสนอภาพรวมที่ครอบคลุมและมีหลักฐานเชิงประจักษ์สำหรับการวินิจฉัย การจัดการแบบไม่ผ่าตัด และการฟื้นฟูสมรรถภาพของผู้ใหญ่ที่มีภาวะเอ็นกล้ามเนื้อหมุนหัวไหล่เสื่อม (RCT) บทความนี้สรุปการอัปเดตที่สำคัญและข้อควรทราบจากแนวทางปี 2025 เพื่อช่วยให้แพทย์สามารถนำไปใช้ได้อย่างมั่นใจและชัดเจนในการปฏิบัติประจำวัน
The 2025 Clinical Practice Guideline delivers a comprehensive and evidence-based overview for the diagnosis, non-surgical management, and rehabilitation of adults with rotator cuff tendinopathy.
Why This Guideline Matters
พัฒนาโดยทีมผู้เชี่ยวชาญระดับนานาชาติจากสาขาการกายภาพบำบัด ศัลยกรรมกระดูก และเวชศาสตร์ฟื้นฟู แนวทางปฏิบัติทางคลินิกนี้ได้รับการพัฒนาขึ้นบนพื้นฐานของการทบทวนวรรณกรรมอย่างเป็นระบบ การมีส่วนร่วมของผู้ป่วย และมาตรฐานวิธีการที่เข้มงวด ได้รับการสนับสนุนจากเครือข่ายการฟื้นฟูสมรรถภาพควิเบก (REPAR), เครือข่ายวิจัยความเจ็บปวดควิเบก (QPRN), และสถาบันกายภาพบำบัดกระดูกและข้อ (AOPT) แห่งสมาคมกายภาพบำบัดอเมริกัน (APTA), ได้รวบรวมหลักฐานที่ดีที่สุดที่มีอยู่สำหรับนักคลินิกทั่วโลก ด้วยตัวแทนผู้ป่วยแปดคนจากสามประเทศที่มีส่วนร่วมในกระบวนการปรับปรุงแนวทางนี้ แนวทางนี้ยังสะท้อนถึงประสบการณ์จริงและความชอบของผู้รับการดูแลอีกด้วย
Evidence Grades Explained
คำแนะนำแต่ละข้อในแนวทางปฏิบัติทางคลินิกจะได้รับการกำหนดระดับชั้นที่สะท้อนถึงความเข้มแข็งและความแน่นอนของหลักฐานที่สนับสนุน:
- Grade A – Strong evidence: Supported by multiple high-quality randomized controlled trials (RCTs) or systematic reviews.
- Grade B – Moderate evidence: Supported by at least one high-quality RCT or several lower- quality RCTs or cohort studies.
- Grade C – Weak evidence: Based on single studies of lower quality or expert consensus where research is limited.
- Grade D – Conflicting evidence: Studies disagree in their findings.
- Grade E – Theoretical/foundational: Based on cadaveric, biomechanical, or animal research.
- Grade F – Expert opinion: Based on best practices and clinical consensus in the absence of empirical evidence.
อาการปวดไหล่ที่เกี่ยวข้องกับเอ็นหมุนไหล่
Gain the confidence and expertise to effectively manage rotator cuff-related shoulder pain in your patients with Filip Struyf. You’ll be equipped with the tools and knowledge to enhance shoulder function, reduce pain, and improve quality of life for your patients.

Key Clinical Recommendations
1. Assessment & Diagnosis
- ประวัติอาการโดยละเอียด (เกรด F): แพทย์ผู้รักษาต้องรวบรวมประวัติผู้ป่วยอย่างละเอียด โดยพิจารณาถึงอายุ เพศ ความถนัดในการใช้มือ ความต้องการในการทำงาน กิจกรรมกีฬา การใช้ยา โรคประจำตัว ปัจจัยทางจิตสังคม กลไกการบาดเจ็บ การรักษาที่ผ่านมา อาการปัจจุบัน (อาการปวด ข้อจำกัดของช่วงการเคลื่อนไหว [ROM] ความอ่อนแรง) และเป้าหมายของผู้ป่วย
- การประเมินทางกายภาพ (เกรด F): ควรรวมถึงการตรวจสอบความผิดปกติ การฝ่อลีบของกล้ามเนื้อ และอาการบวม การวัดช่วงการเคลื่อนไหวแบบแอคทีฟ/พาสซีฟและความแข็งแรง การคลำและทดสอบพิเศษเพิ่มเติมตามดุลยพินิจทางคลินิก ควรตรวจกระดูกสันหลังส่วนคอเพื่อแยกความเจ็บปวดที่ส่งต่อ
- ธงแดง (เกรด F): แพทย์ต้องคัดกรองโรคที่รุนแรง เช่น การติดเชื้อ มะเร็ง โรคทางหัวใจและหลอดเลือด หรือการลุกลามของโรคในระบบต่าง ๆ ของร่างกาย ปัจจัยพยากรณ์ (ระดับ B): แนะนำให้ระบุปัจจัยส่วนบุคคล ปัจจัยทางคลินิก และปัจจัยที่เกี่ยวข้องกับการทำงานที่มีผลต่อการพยากรณ์โรค เพื่อเป็นแนวทางในการจัดทำแผนการดูแลเฉพาะบุคคล
- การทดสอบพิเศษ (เกรด B): การทดสอบโค้งที่เจ็บปวดสามารถช่วยยืนยันการวินิจฉัยได้ ในขณะที่การทดสอบฮอว์กินส์-เคนเนดีสามารถช่วยในการคัดกรองได้
- การวัดเชิงวัตถุประสงค์ (เกรด A): ROM ควรวัดโดยใช้กอนิโอมิเตอร์, อินคลิโนมิเตอร์, หรือแอปพลิเคชันสมาร์ทโฟนที่ได้รับการตรวจสอบความถูกต้อง. การวัดช่วงการเคลื่อนไหวของกระดูกสะบักไม่น่าเชื่อถือและไม่แนะนำให้ใช้ การทดสอบความแข็งแรงควรดำเนินการโดยใช้เครื่องวัดแรงแบบมือถือ
- มาตรการผลลัพธ์ที่รายงานโดยผู้ป่วย (เกรด A): ใช้เครื่องมือที่ได้รับการตรวจสอบแล้วว่าเชื่อถือได้และตอบสนองได้ดี เช่น แบบประเมินความเจ็บปวดและภาวะทุพพลภาพของไหล่ (SPADI) หรือแบบสอบถามภาวะทุพพลภาพของแขน ไหล่ และมือ (DASH) เพื่อติดตามความเจ็บปวดและภาวะทุพพลภาพ
- การถ่ายภาพ (เกรด F): ไม่ควรใช้ในตอนแรก การตรวจอัลตราซาวด์เพื่อการวินิจฉัยควรได้รับการพิจารณาหากจำเป็นต้องมีการถ่ายภาพหลังจากการดูแลแบบอนุรักษ์นิยมล้มเหลวเป็นเวลา 12 สัปดาห์ การถ่ายภาพด้วยคลื่นแม่เหล็กไฟฟ้า (MRI) ไม่แนะนำให้ทำเป็นประจำ พูดคุยข้อดี/ข้อเสียของการถ่ายภาพทางการแพทย์กับผู้ป่วยอย่างเปิดเผย
- การส่งต่อ (ระดับ F): ผู้ป่วยที่มีอาการคงอยู่และรุนแรงหลังการรักษาเป็นเวลา 12 สัปดาห์ ควรส่งต่อไปยังผู้เชี่ยวชาญด้านระบบกล้ามเนื้อและกระดูก (เช่น แพทย์เวชศาสตร์การกีฬา แพทย์เวชศาสตร์ฟื้นฟู หรือศัลยแพทย์กระดูกและข้อ)
2. Pharmacological Treatment
- Acetaminophen (Grade C): May be recommended for short-term pain relief. Non-Steroidal
- Anti-Inflammatory Drugs (NSAIDs) (Grade B): Effective for short-term pain management.
- Opioids (Grades F/C): Should not be used as first-line treatment. May be considered short-term in severe cases where other options are ineffective or contraindicated. Requires regular risk reassessment.
- การฉีดคอร์ติโคสเตียรอยด์ (เกรด B/C): อาจใช้สำหรับบรรเทาอาการปวดระยะสั้น แต่ไม่ควรใช้เป็นการรักษาเบื้องต้น แนะนำให้ใช้การนำทางด้วยอัลตราซาวด์หากมีการฉีดยา
- การล้างแคลเซียม (เกรด B): แนะนำสำหรับโรคเอ็นเสื่อมที่มีการสะสมของแคลเซียมที่ไม่ตอบสนองต่อการรักษาเบื้องต้น
- Platelet-Rich Plasma (PRP) & Hyaluronic Acid (Grades D/F): May be considered
3. Rehabilitation Principles
- การศึกษา (เกรด C): แพทย์ควรให้การศึกษาแก่ผู้ป่วยเกี่ยวกับโรคของพวกเขา, การปรับเปลี่ยนกิจกรรม, ความรู้ทางประสาทวิทยาเกี่ยวกับความเจ็บปวด, การคาดการณ์, และกลยุทธ์การจัดการตนเอง. ปรับการสื่อสารให้เหมาะสมกับระดับความรู้และการรับรู้ทางสังคมและจิตวิทยา
- การบำบัดด้วยการออกกำลังกาย (เกรด A): การแทรกแซงหลัก ควรรวมการฝึกความต้านทานแบบก้าวหน้าและการออกกำลังกายควบคุมการเคลื่อนไหว ปรับให้เหมาะสมเป็นรายบุคคลตามระดับความทนต่อความเจ็บปวดและเป้าหมายของผู้ป่วย
- การบำบัดด้วยมือ (เกรด B): อาจช่วยลดอาการปวดในระยะสั้นเมื่อใช้ร่วมกับการออกกำลังกาย เทคนิคประกอบด้วยการทำงานกับเนื้อเยื่ออ่อนและการเคลื่อนไหว/การจัดกระดูกข้อต่อ
- Taping (Grade D): Can be used adjunctively to reduce pain short-term.
- การฝังเข็ม (เกรด C): อาจให้ประโยชน์เพิ่มเติมในระยะสั้นเมื่อใช้ร่วมกับการฟื้นฟูสมรรถภาพเชิงรุก
- การบำบัดด้วยคลื่นกระแทก (เกรด C): มีประโยชน์ในภาวะเอ็นเสื่อมจากการสะสมของแคลเซียม ไม่แนะนำให้ใช้ใน RCT ที่ไม่มีการสะสมแคลเซียม
- Laser Therapy (Grade C): May reduce pain in calcific tendinopathy.
- อัลตราซาวนด์บำบัด (เกรด C/B): ไม่แนะนำให้ใช้สำหรับ RCT ที่มีแคลเซียมหรือไม่มีแคลเซียม เนื่องจากไม่มีประโยชน์
- Ergonomic Modifications (Grade C): May help reduce occupational stress on the shoulder.
4. Return to Sport
- ความทนทานต่อการโหลด (เกรด F): แผนการกลับมาเล่นกีฬาควรมีพื้นฐานจากความสามารถของนักกีฬาในการทนต่อการรับน้ำหนักของไหล่และกล้ามเนื้อหมุนหัวไหล่
- มาตรการผลลัพธ์ (เกรด F): ใช้เครื่องมือที่ได้รับการตรวจสอบแล้วเพื่อประเมินความเจ็บปวด, ความพิการ, ความพร้อมในการกลับมา, และสมรรถภาพการทำงาน. ตัวอย่างได้แก่ การทดสอบสมรรถภาพเฉพาะทางกีฬา และรายการตรวจสอบการกลับมาเล่นกีฬา
สรุป
แนวทางการปฏิบัติทางคลินิกสำหรับโรคเอ็นกล้ามเนื้อหมุนหัวไหล่อักเสบ ปี 2025 นำเสนอแนวทางที่ชัดเจนและครอบคลุมสำหรับการดูแลรักษาไหล่แบบอนุรักษ์นิยม ให้ความสำคัญกับการประเมินเฉพาะบุคคลโดยอิงจากประวัติผู้ป่วยและการตรวจร่างกายทางคลินิก ไม่แนะนำให้ใช้การถ่ายภาพรังสีในระยะแรก และสนับสนุนการใช้เครื่องมือวัดเชิงวัตถุสำหรับช่วงการเคลื่อนไหวและความแข็งแรง การแทรกแซงทางเภสัชวิทยาเป็นเพียงการเสริมในการฟื้นฟูสมรรถภาพเชิงรุก โดยมีกายภาพบำบัดเป็นรากฐานสำคัญของการฟื้นฟู การบำบัดเสริม เช่น การบำบัดด้วยมือ การพันเทป และการฝังเข็ม อาจพิจารณาใช้เป็นบางกรณี แนวทางนี้ยังเน้นย้ำถึงความสำคัญของการศึกษาที่มุ่งเน้นผู้ป่วยเป็นศูนย์กลางและการจัดทำโปรแกรมการกลับมาเล่นกีฬาแบบค่อยเป็นค่อยไปโดยคำนึงถึงปริมาณการฝึก โดยรวมแล้ว สิ่งนี้ส่งเสริมให้แพทย์พึ่งพาการถ่ายภาพทางการวินิจฉัยและวิธีการแบบพาสซีฟน้อยลง และให้ความสำคัญกับกลยุทธ์เชิงรุกที่อิงหลักฐานและเสริมพลังให้ผู้ป่วยมากขึ้น
Changes from the 2022 guideline:
- Integration of systematic reviews up to October 2023.
- New recommendations specifically addressing return to sport.
- Clearer grading of evidence using GRADE-adapted methodology.
- Enhanced patient-centered language and prioritization of shared decision-making.
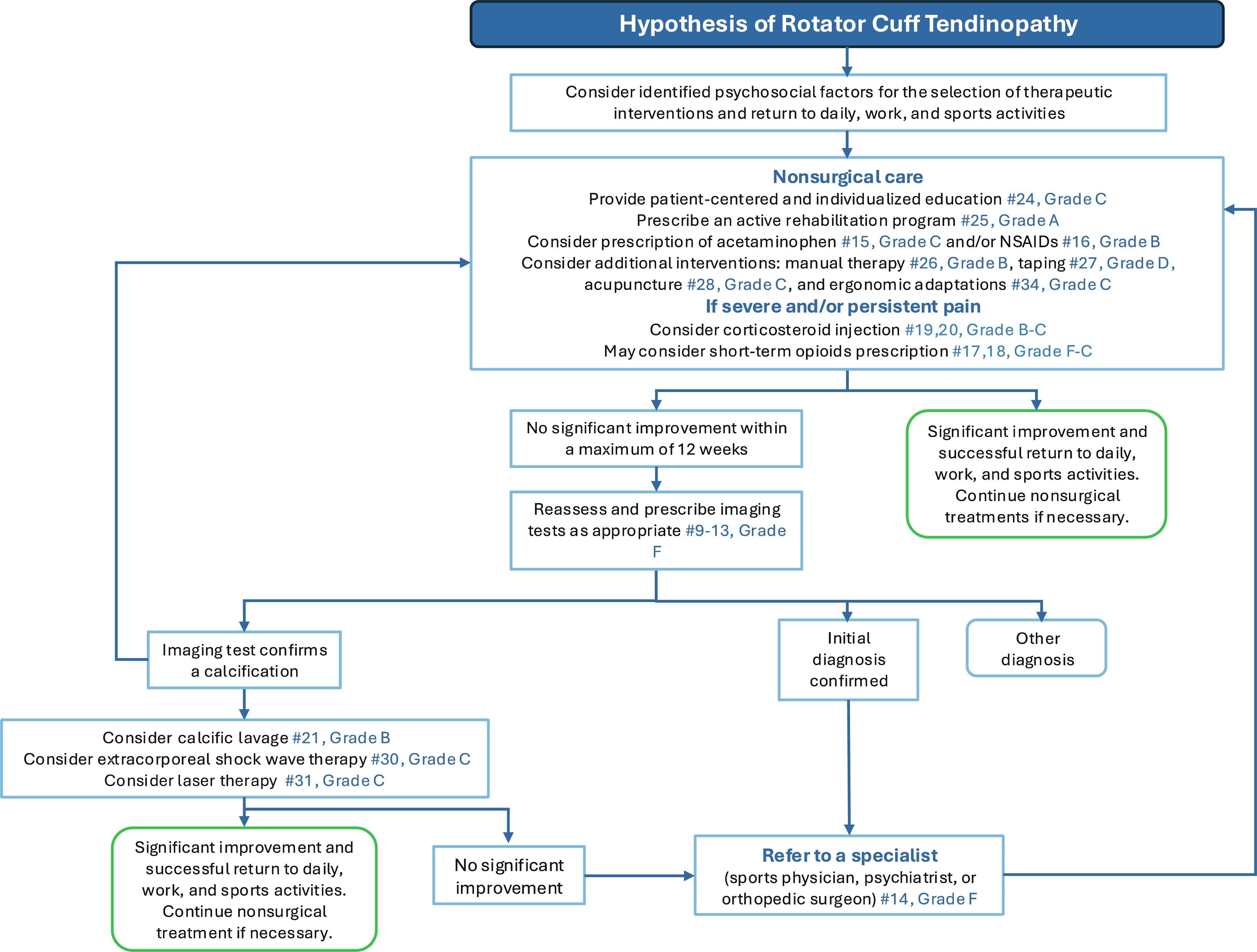
The Rotator Cuff Management Decision Tree
ผู้เขียนได้จัดทำแผนผังการตัดสินใจเพิ่มเติมเพื่อเป็นแนวทางให้แพทย์ในการดูแลผู้ป่วยในกระบวนการฟื้นฟูจากภาวะเอ็นกล้ามเนื้อหมุนหัวไหล่อักเสบ
Limitations & Conclusion
แม้ว่าแนวทางนี้จะมีรายละเอียดครอบคลุม แต่บางประเด็น เช่น ระยะเวลาในการกลับไปเล่นกีฬาและประสิทธิผลของการใช้พลาสม่าเข้มข้นเกล็ดเลือด ยังขาดการศึกษาวิจัยแบบสุ่มที่มีคุณภาพสูง จำเป็นต้องมีการวิจัยเพิ่มเติมเพื่อปรับการรักษาให้เหมาะสมกับแต่ละบุคคลและระบุกลุ่มย่อยที่มีพยากรณ์โรคแตกต่างกัน แนวทางเวชปฏิบัติปี 2025 สำหรับโรคเอ็นกล้ามเนื้อหมุนหัวไหล่เสื่อม (Rotator Cuff Tendinopathy) นำเสนอแนวทางที่มีหลักฐานเชิงประจักษ์และยึดผู้ป่วยเป็นศูนย์กลาง ซึ่งสามารถลดการรักษาเกินความจำเป็นและปรับปรุงผลลัพธ์ทางคลินิกได้ โดยการปรับการปฏิบัติให้สอดคล้องกับคำแนะนำเหล่านี้ แพทย์สามารถประเมิน ให้ความรู้ และฟื้นฟูผู้ใหญ่ที่มีภาวะ RCT ได้อย่างมั่นใจมากขึ้น
อ้างอิง
เดสมูเลส์, เอฟ., รอย, เจ-เอส., ลาฟรองซ์, เอส., และคณะ. (2025). การวินิจฉัยโรคเอ็นกล้ามเนื้อหมุนหัวไหล่อักเสบ, การดูแลทางการแพทย์แบบไม่ผ่าตัด และการฟื้นฟูสมรรถภาพ: แนวทางการปฏิบัติทางคลินิก วารสารกายภาพบำบัดออร์โธปิดิกส์และกีฬา https://doi.org/10.2519/jospt.2025.13182

กุส โรธูอิเซ่น
บทความบล็อกใหม่ในกล่องจดหมายของคุณ
สมัครสมาชิกตอนนี้ และรับการแจ้งเตือนเมื่อมีการเผยแพร่บทความบล็อกล่าสุด





