ผลการป้องกันของการเคลื่อนไหวระบบประสาทต่ออาการปวดกล้ามเนื้อหลังออกกำลังกาย (DOMS)

การแนะนำ
Delayed onset muscle soreness (DOMS) is a well-known phenomenon that occurs after (strength) training. It is thought to originate from local exercise-induced muscle damage and subsequent local inflammation. Although DOMS is a temporary condition, it can negatively affect training, participation in activities, and may deter others from engaging in training and exercise. As the local inflammatory response, which results from the exercise-induced microdamage within the muscles, releases proinflammatory cytokines, the sensitivity of the peripheral nerve endings is increased, resulting in pain.
Neurodynamic mobilizations have been extensively studied in nerve-related conditions (Lascurain-Aguirrebeña et al. 2024) and found to enhance axonal transport in the nerve and surrounding tissues, facilitating the distribution of local inflammatory mediators. By this improved axonal transport, the local inflammatory response can be regulated. As DOMS results in a local inflammatory response due to local intraneural edema, the authors from this study hypothesized that an intervention with neurodynamic mobilizations can improve axonal transport and support synaptic plasticity, thereby reducing peripheral nerve inflammation and subsequently, pain from DOMS as well. Therefore, the preventive effects of neurodynamic mobilizations on DOMS were investigated.
วิธีการ
A prospective single-blind randomized, placebo-controlled trial was conducted in Turkey. Young, untrained, healthy but sedentary men between 20 and 32 years of age were included. According to the American College of Sports Medicine guidelines, a sedentary lifestyle was defined as engaging in less than 30 minutes of physical activity for five days a week.
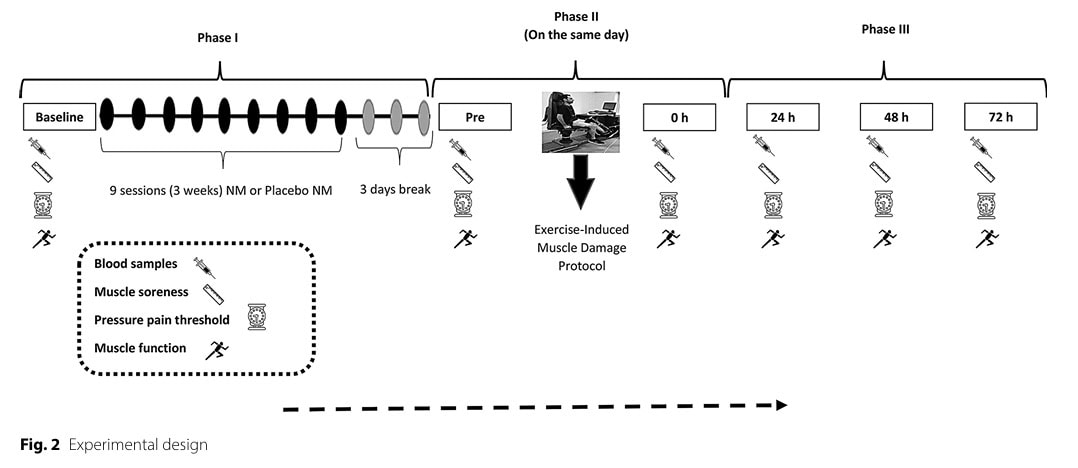
The study was subdivided into three phases:
- Phase 1:
- Baseline collection of data on muscle soreness, pressure pain threshold (PPT), and one-leg hop test for distance as a muscle function test. Blood samples were collected.
- Nine sessions of neurodynamic mobilizations or placebo neurodynamic mobilizations were performed over three weeks. Three sets of 10 repetitions were completed at every session, with 2-minute intervals between the sets.
- Phase 2:
- After a 3-day break, phase 2 started with repeating the collection of blood samples and data on muscle soreness and function, and PPTs
- Participants from the intervention group and the placebo group then participated in an exercise-induced muscle damage (EIMD) protocol on a dynamometer device.
- Immediately after the eccentric exercise, all measurements were repeated.
- Phase 3 collected all blood samples and measurements of muscle soreness and function, and PPTs at 24h, 48h, and 72h after the EIMD protocol.
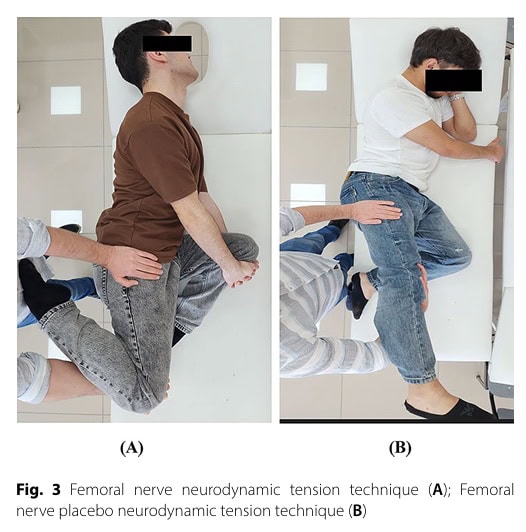
In the intervention group, the neurodynamic mobilization was performed with the participants lying on their non-dominant sides. With the therapist standing behind the participant, the upper leg was brought into knee flexion and supported with the hip in a neutral position. Then the leg was extended at the hip joint until the participant reported soreness or pain. This tensioning position was maintained for 3 seconds. In every session, 3 sets of 10 repetitions were performed with 2-minute breaks in between sets.
The placebo group received a slightly modified neurodynamic mobilization in the same side-lying position. The procedure was performed similarly, except that no knee flexion was performed during the technique.
The exercise-induced muscle damage protocol consisted of 30 sets of 10 eccentric contractions, which were performed for the dominant quadriceps femoris muscle at 30° per second, between 35° and 95° of flexion. Participants were instructed to extend their leg as if kicking a ball as hard as they could (for the knee extensors) and resist the upward motion from the machine (for the knee flexors).
Following outcome measures were collected:
- Muscle soreness on a 0-100 visual analogue scale while going down the stairs.
- Pressure pain threshold (PPT), measured 5 cm proximal to the superior border of the patella. A digital pressure algometer was used.
- Muscle function was quantified using the one-leg hop for distance test, with a mean of 3 attempts.
- Blood samples were collected and analyzed for biomarkers of muscle damage (creatine kinase (CK) and lactate dehydrogenase (LDH)) and inflammation (tumor necrosis factor-alpha (TNF-a) and human interleukin-6 (IL-6)).
ผลลัพธ์
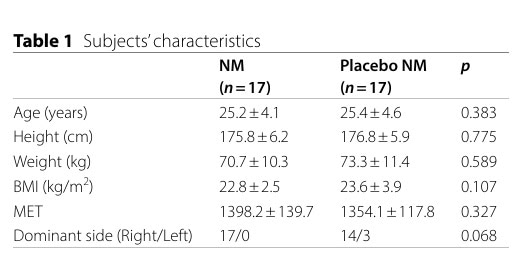
Thirty-four adults were included in the analyses and were equally randomized into the intervention group receiving the neurodynamic mobilization or in the placebo group. Their baseline characteristics revealed no differences in demographics between the groups.
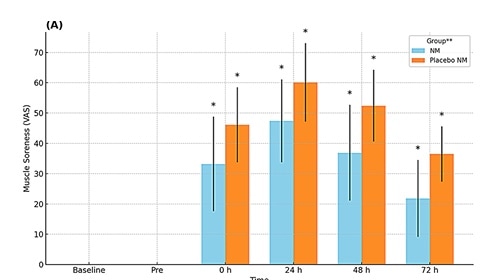
To study the preventive effects of neurodynamic mobilizations on DOMS, the authors compared both groups after the exercise-induced muscle damage protocol. For the outcome muscle soreness, a significant time x group effect was observed. Muscle soreness peaked at 24 hours following the exercise protocol. The placebo group experienced more muscle soreness (+47%) compared to the intervention group (+60%) at 24h. The same preventive effect of neurodynamic mobilizations on DOMS was found at 48h and 72h.
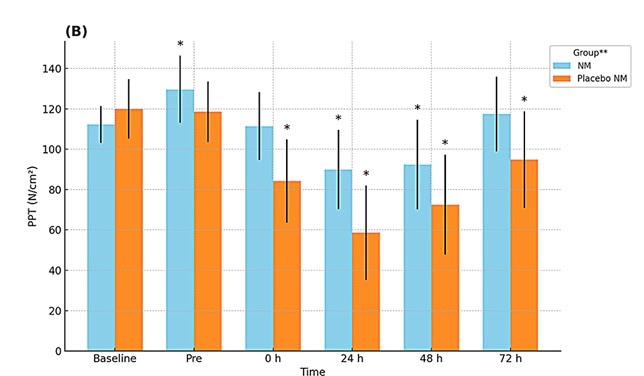
Also, regarding the pressure pain threshold (PPT), a significant time x group effect was observed after the exercise protocol. The PPT reached its lowest value 24 h after the exercise-induced muscle damage protocol in both groups. Yet, there was also a preventive effect of the neurodynamic mobilizations on DOMS in the intervention group. The placebo group had a larger decrease in PPT (-52%) than the intervention group (-20%) compared with the baseline. The intervention group had significantly higher PPTs at 24h, 48h, and 72h following the exercise-induced muscle damage protocol. Additionally, the intervention group returned to their baseline PPT value at 72h following the exercise protocol, whereas the placebo group had not yet returned to their baseline PPT.
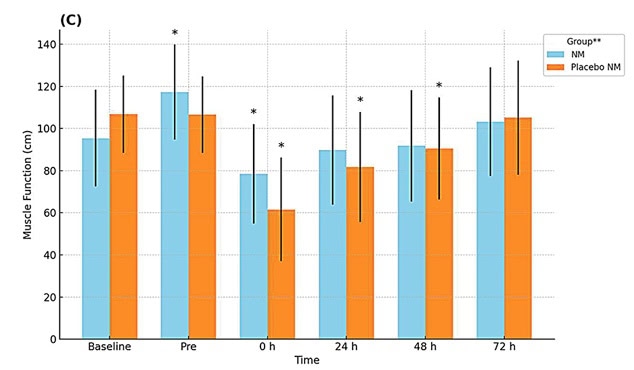
For the outcome of muscle function, a significant time x group effect also emerged. In both groups the scores were lowest immediately after the exercise-induced muscle damage protocol, however the scores were lower in the placebo group (-41%) compared to the intervention (-18%). The intervention group also performed better before the exercise protocol (after the neurodynamic mobilization protocol) compared to the placebo group, where there was no difference at baseline. Remarkably, the intervention group returned to their baseline muscle function at 24h following the exercise-induced muscle damage protocol compared to the placebo group where it took 72h.
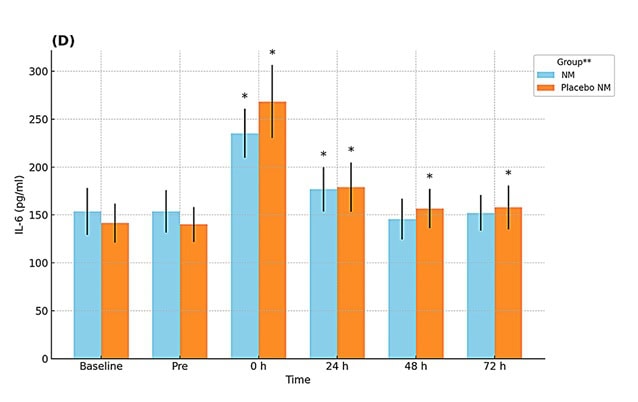
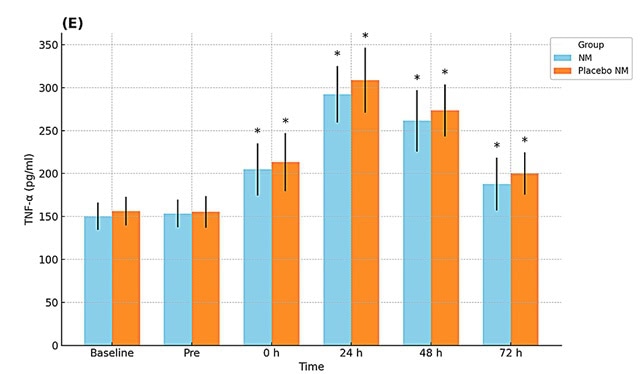
The effects on the inflammatory markers demonstrated a significant time x group interaction for IL-6, and only a significant time effect for TNF-a. Immediately after the exercise protocol, IL-6 peaked, and TNF-a reached its peak at 24h. Both groups showed increases in IL-6 and TNF-a, but regarding the IL-6 values, the intervention group had less increase (+53% versus +90%) immediately after the exercise protocol. IL-6 values returned to baseline values at 48h in the intervention group, whereas in the placebo group this was still not the case at 72h.
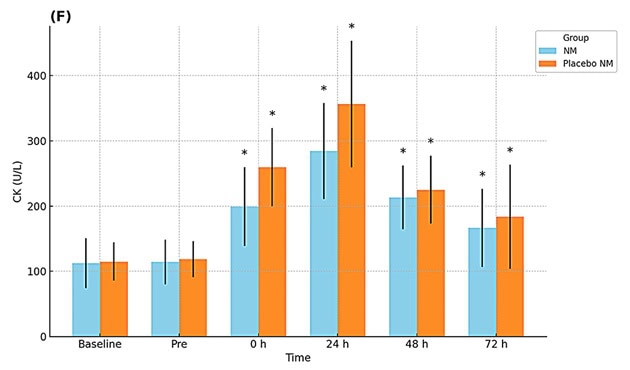
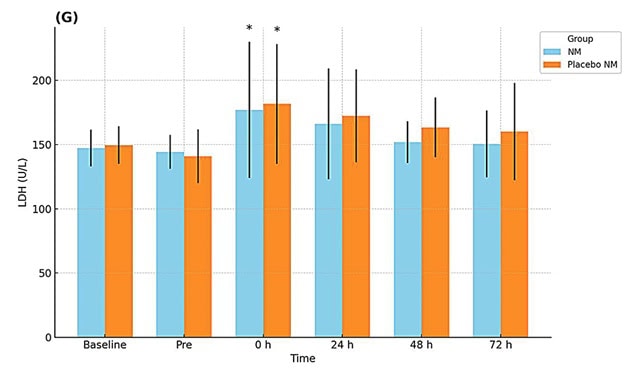
Markers of muscle damage showed no significant group x time effects, only a time effect was observed. A significant between-group difference was found only for CK concentrations at 0 h and 24 h.
คำถามและความคิด
The preventive effect of neurodynamic mobilizations on DOMS was partially supported by this study’s findings. While the functional muscle test, the muscle soreness test and the pain pressure threshold were markedly different between the two groups, only the IL-6 biomarker supported the clinical findings. For TNF-a, CK and LDH no significant differences between the groups emerged. While CK and LDH are biomarkers of muscle damage, they are not exclusively related to muscle breakdown. For instance, people with hypothyroidism can also show elevated blood serum levels of CK (Hemavathi et al. 2016).
Also, DOMS is not exclusively a sign of muscle damage as it also encompasses an inflammatory response secondary to the local microtraumata within the muscles. This local inflammatory response triggers a cascade of effects where local edema and sensitization of local nerve endings occur, contributing to the pain experience (Peake et al. 2017).
The present study was the first to investigate the potential protective effects of neurodynamic mobilizations on DOMS and revealed interesting findings regarding the potential role of nervous system-focused strategies. Since sensitization of nerve endings occurs, the influence of neurodynamic mobilizations on DOMS may explain the observed pain modulation.
In my opinion, the use of neurodynamic mobilizations as a preventive strategy for reducing the adverse effects like DOMS can be an interesting pathway to encourage older and less experienced people to participate in adequately dosed-exercise. Although further research is necessary to confirm the current results and improve the limitations of this paper,
It would be informative to investigate what dosage is needed to reduce DOMS. In this study, a total of 9 sessions were conducted. Since only 3 sets of 10x 3-second repetitions were performed with 2-minute breaks between sets, it may be an effective tool to reduce DOMS. However, is it necessary to perform several weeks of these neurodynamic mobilization sessions before starting intensive training? Can a combination of these neurodynamic mobilizations at the beginning of a training session be sufficient for some people who are less experienced in strengthening or should it be delayed for a period of time after receiving these mobilizations? Can it be regarded as a prehab strategy? However, many questions remain unanswered, which is normal for a first study concerning this topic
พูดจาเนิร์ดกับฉันสิ
The protocol of this experimental study was retrospectively registered, but no reasons were provided. The trial registry pointed out that several modifications to the trial were done, for example, a ROM assessment was removed. Furthermore, no primary outcome measure was specified, and multiple outcomes were analyzed without a Bonferroni correction applied. This altogether limits the study in drawing firm conclusions despite the use of a randomized controlled design. Future studies should further investigate the findings.
A concerning limitation is the absence of a blinded outcome assessor. Based on the information provided in the study, a fully blinded outcome assessor was NOT involved. Only the participants were blinded, as the study was conducted as a randomized, single-blind study. While participants were blinded to their group assignment, the researcher who conducted the assessments was not. This means that the researchers measuring the outcomes (muscle soreness, PPT, muscle function, blood samples, etc.) were aware of which group each participant belonged to. This lack of blinding for the outcome assessor introduces a significant potential for bias.
It should be noted that this was a young but sedentary population and that these results can not directly be translated into other more athletic or older populations. Similarly, the exercise-induced muscle soreness is an experimentally-induced form of DOMS, which may not fully replicate DOMS that occurs under natural conditions. This could limit the real-world applicability of the findings.
While the preventive effect of neurodynamic mobilizations on DOMS was only partially supported, the effect on the one-leg jump for distance is relatively straightforward. The intervention group receiving the neurodynamic mobilizations had less decrease in performance in the one-leg jump for distance test. The authors propose that their intervention possesses a mechanism for modulating muscle damage and inflammatory responses induced by DOMS.
Take-home messages
This study investigated the preventive effects of femoral nerve neurodynamic mobilizations on DOMS. The intervention was applied for three weeks prior to exercise-induced muscle damage and compared to placebo. The intervention had positive effects on reducing muscle soreness, increasing pressure pain threshold (PPT), improving muscle function, and lowering Interleukin-6 (IL-6) levels, but did not show preventive effects on other muscle damage and inflammatory parameters. This suggests that neurodynamic mobilizations may help alleviate inflammation and muscle damage symptoms and shorten recovery time following DOMS, but further research with larger and diverse groups is needed.
อ้างอิง
สิ่งที่ต้องระวังเพื่อป้องกันการบาดเจ็บของกล้ามเนื้อต้นขาด้านหลัง น่อง และต้นขาด้านหน้า
ไม่ว่าคุณจะทำงานร่วมกับนักกีฬาระดับสูงหรือมือสมัครเล่น คุณคงไม่อยากพลาดปัจจัยเสี่ยงเหล่านี้ ซึ่งอาจทำให้พวกเขามีความเสี่ยงต่อการบาดเจ็บที่สูงกว่าได้ เว็บสัมมนาครั้งนี้จะ ช่วยให้คุณระบุปัจจัยเสี่ยงต่างๆ เพื่อแก้ไขในระหว่างการฟื้นฟู!

