Rehabilitering av sensorimotorisk dysfunksjon ved korsbåndskader

Introduksjon
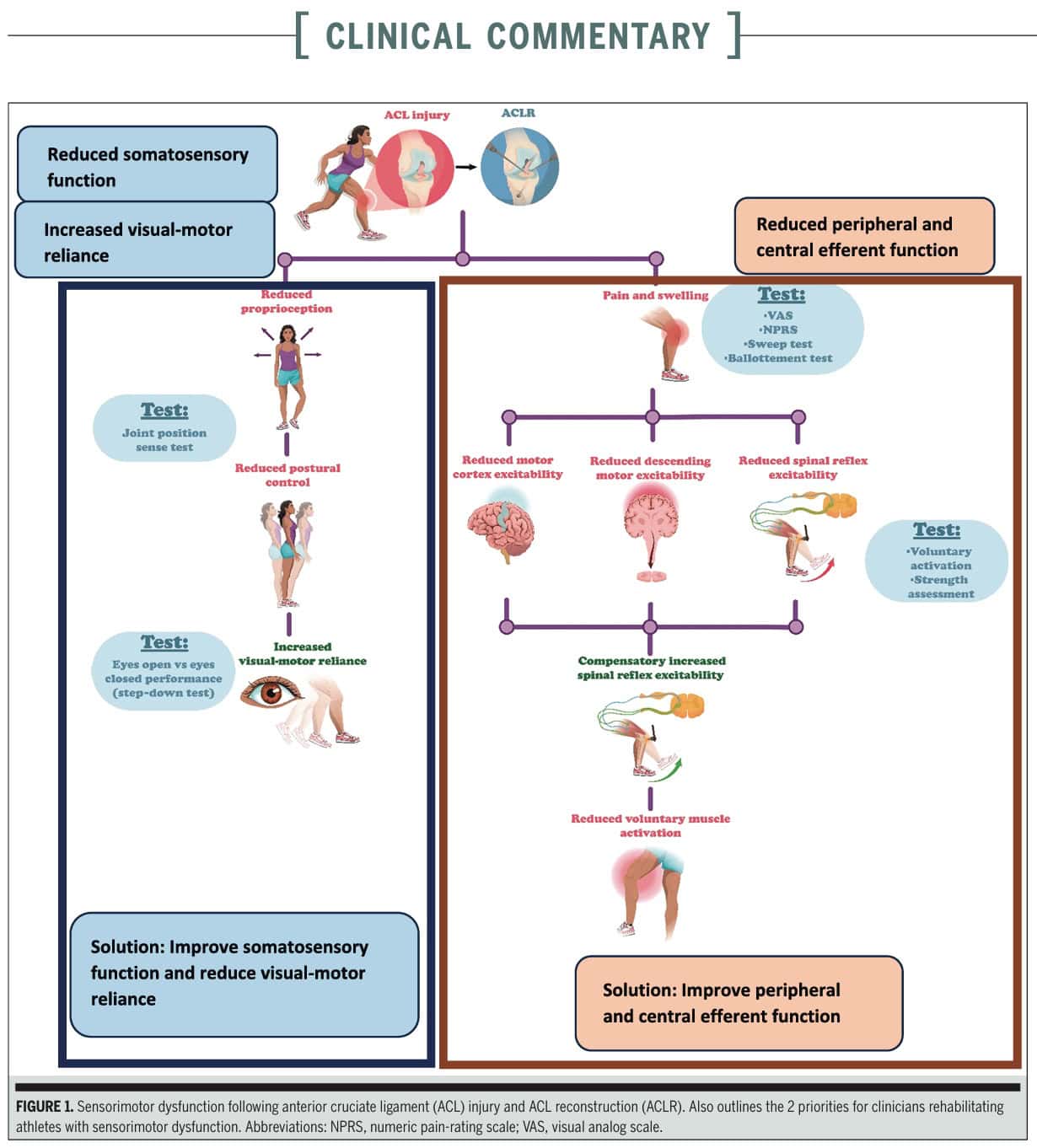
Sensorimotor dysfunctions are common following ACL injuries and can persist for a long time, even after reconstruction and rehabilitation, contributing to a high reinjury risk if left unaffected. This study is the second part of the clinical commentary by Vitharana et al. (2025), which we covered in an earlier research review. While Part 1 focused on assessing the presence of sensorimotor dysfunctions in ACL injuries, this part focuses on how sensorimotor dysfunction rehabilitation of ACL injuries should happen.
Metoder
By reviewing the evidence around sensorimotor dysfunction rehabilitation of ACL injuries, the authors want to provide you with the knowledge to identify (Part 1) and rehabilitate these dysfunctions. This paper is written as a clinical commentary that includes a systematic approach to reviewing the literature to inform clinical practice. It is, however, not a formal systematic review with a meta-analysis of primary studies, which adheres to more rigorous statistical and methodological criteria.
The authors propose two main priorities for sensorimotor dysfunction rehabilitation of ACL injuries to effectively manage sensorimotor dysfunction
- Improving the peripheral and central efferent function: This focuses on the pathways that take neural activity to the muscles for movement, including activity within the brain and descending motor pathways
- Improving somatosensory function and reducing reliance on the visual-motor system: This addresses issues with sensing body position (proprioception), movement, touch, pressure, and pain, as well as the tendency for individuals with ACL injuries to rely more on vision for movement.
Resultater
The clinical commentary outlined the following key priorities for sensorimotor dysfunction rehabilitation of ACL injuries.
- Improving Peripheral and Central Efferent Function:
In the Early-Stage Rehabilitation, which is the first few weeks post-injury/surgery, the pain and swelling lead to a reduction in spinal reflexive and motor cortex excitability, which in turn leads to reduced voluntary activation of the quadriceps and loss of strength and proprioception. Therefore, the priority is to manage pain and swelling around the knee.
The authors propose the following modalities to help reduce the swelling and pain:
- Regular movement of the knee
- Lower-limb strength exercises
- Gait retraining
Additionally, the authors indicate the following modalities
- Nonsteroidal anti-inflammatory medications and analgesics can be helpful, especially in the first 3 days post-operative period, where the pain is typically worse. This should be prescribed by the treating physician or surgeon. Sometimes, a nerve block is carried out by the surgeon to reduce postoperative pain and analgesic use.
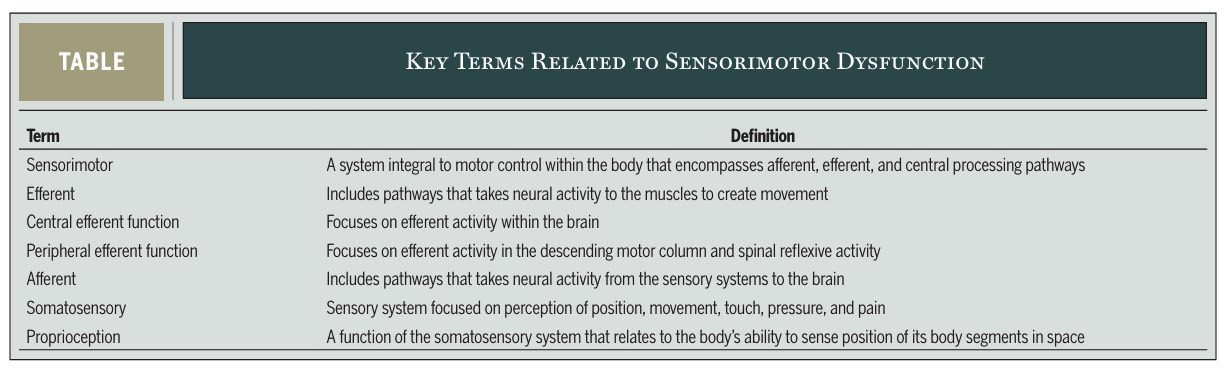
- Transcutaneous Electrical Nerve Stimulation (TENS) can be an alternative for analgesic medications, since it stimulates large-diameter afferent nerve fibers, which are processed in the cortex and stimulate descending inhibitory pathways. The article recommends using TENS for 20 minutes in at least 5 treatment sessions. A stimulus at low (1-8 Hz) or high (2-120 Hz) frequencies is recommended.
- The use of cryotherapy (with or without compression devices) is another alternative for analgesic medication. It is recommended 3 times a day for the first 6 weeks post-operatively, or at least once daily in case of limited accessibility. Devices like “Game Ready” or “Cryocuff IC Cooler” are more effective than ice packs alone, according to the authors.
Throughout Rehabilitation, following the first weeks, strength training should be the cornerstone of the physiotherapy sessions. Strength training is an effective stimulus to improve peripheral and central efferent function.
- Training at the right intensity is crucial. Progressive strength training at >75% of 1 repetition maximum (1RM) significantly increases corticospinal excitability, while lower intensities (25% 1RM) show no changes, according to Welling et al. (2019). A resistance program with progressive overload (to >90% 1RM) has been shown to achieve symmetrical strength compared to healthy controls by 7 months post-surgery.
- Neuromuscular Electrical Stimulation (NMES) can be used as an adjunct to strength training. NMES stimulates efferent function, with minimal loading of the knee joint, and is, therefore, especially helpful in the early phases. The authors recommend using NMES with contraction times of 15-20 seconds and rest times of 15-50 seconds. Studies report the use of NMES, especially in the first 5-7 days per week for the first 4-12 weeks. Thereafter, it can be used on non-strength training days or as part of a warm-up (5-10 minutes) in later stages.
- Another adjunct to strength training is the use of surface Electromyography (EMG) Biofeedback. EMG devices measure motor unit recruitment and provide visual/auditory feedback to the athlete about their contraction. As it provides an external focus, it improves corticospinal excitability (unlike NMES) and increases quadriceps strength. NMES can be used with isometric and isotonic exercises, for 5-7 days per week, and it can be integrated into strength sessions.
- Improving Somatosensory Function and Reducing Reliance on the Visual-Motor System
Proprioceptive training is essential for early sensorimotor dysfunction rehabilitation of ACL injuries and is recommended within the first 6 weeks of injury/surgery to restore normal function, reduce reinjury risk, and minimize visual-motor reliance.
As the ACL is injured, a decrease or loss of afferent feedback occurs, which contributes to the development of sensorimotor dysfunctions. It is unclear whether the proprioceptive nerve fibers regrow fully into the ACL after injury and how fast this occurs. Therefore, it is especially important to improve proprioception of the surrounding muscles and joints. The underlying mechanism of proprioceptive training focuses on using somatosensory afferent information in the absence of vision.
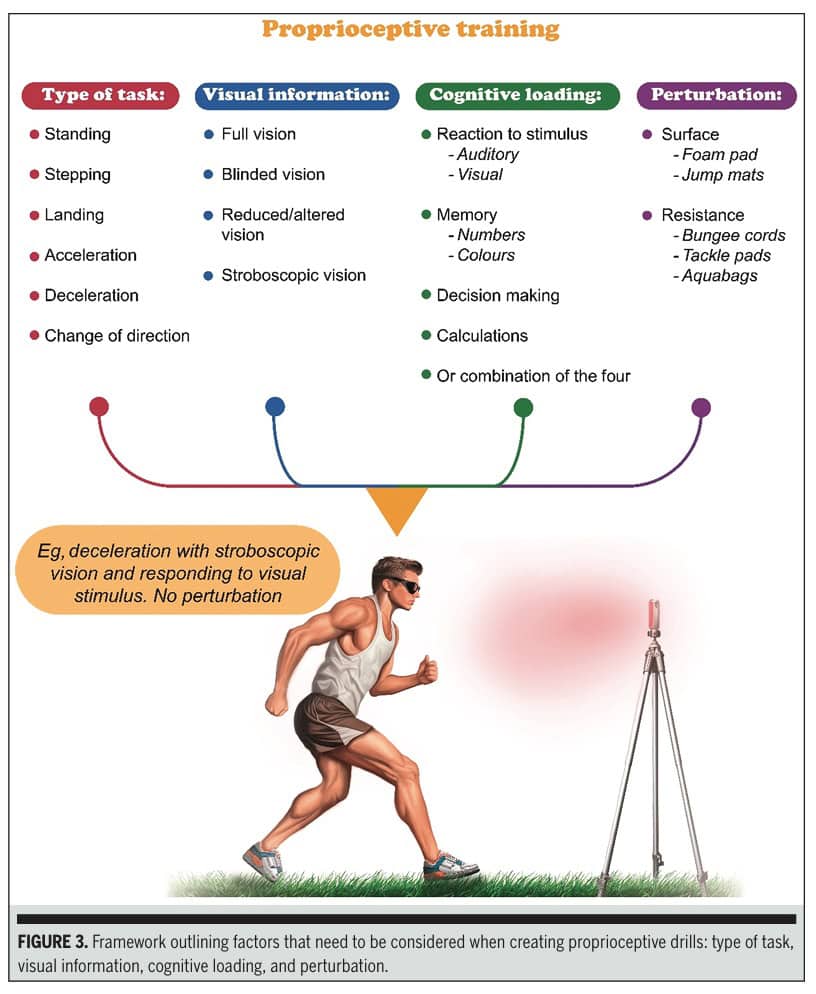
You can start with balance exercises, but you should progressively increase the complexity of the exercises throughout the rehabilitation.
- Progression of Complexity:
- Type of Task: Progress from low-load, low-velocity tasks (e.g., single-leg standing/squatting) to higher loads and velocities in multiple planes (e.g., stepping, landing, deceleration, change-of-direction tasks)
- Visual Information: Reduce visual input. Start with full vision, then blinded vision (eyes closed). For dynamic tasks, stroboscopic glasses
- Cognitive Loading: Add cognitive tasks to proprioceptive drills to simulate chaotic sporting environments. This can include reaction to a stimulus (auditory/visual), memory tasks (numbers/colors), decision-making, or calculations
- Perturbation: Incorporate unexpected forces to induce rapid, sudden motor responses and challenge stability. Examples include foam surfaces, jump mats, bungee cords, tackle pads, or aquabags
Spørsmål og tanker
The clinical commentary did not specifically indicate for which patients and injury characteristics these recommendations served. There may be specific patient populations (e.g., based on age, activity level, presence of comorbidities) for whom these rehabilitation strategies might need to be adapted. Also, injuries can vary a lot, think of concomitant ACL and meniscal injuries, or cartilage defects that may require other rehabilitation strategies at first (non-weight bearing for a certain period, for example). While people having concomitant injuries also have to get rid of the sensorimotor dysfunctions around their knee, the timelines as proposed here can vary.
Physiotherapy rehabilitation treatment also depends on the type of ACL injury (contact versus non-contact), the initial treatment (surgery versus conservative care). The paper uses examples from both surgical and non-surgical cases, but does not specifically differentiate the proposed rehabilitation methods.
The commentary primarily focuses on the physiological aspects of sensorimotor dysfunction rehabilitation of ACL. However, psychological factors such as fear of reinjury, self-efficacy, and motivation play a significant role in rehabilitation outcomes.
Snakk nerdete til meg
While this is a clinical commentary and not a formal systematic review, it serves as an expert opinion publication, synthesizing existing research for clinical application. Its strength lies in providing informative and actionable assessment strategies for sensorimotor dysfunction rehabilitation of ACL injuries, even though it’s a lower level of evidence. This means the recommendations, while evidence-based, may not be as rigorously supported by a comprehensive analysis of all available research.
The authors of the clinical commentary indicated there is a lack of prospective research on proprioceptive training’s ability to reduce visual-motor reliance. So we must be aware that these recommendations may be preliminary and subject to change.
While the impact of ACL injuries on the sensorimotor system is well-documented, more than just the knee is affected. We must be aware that other joints surrounding the affected knee will likely be affected as well, so it is important to broaden your examination to get a better picture of the patient in front of you.
Ta med hjem meldinger
Sensorimotor dysfunction rehabilitation of ACL injuries should focus on improving peripheral and central efferent function and improving somatosensory function while reducing visual-motor reliance. Interventions should be implemented early and progress over time. Strength training, NMES, and surface EMG biofeedback are effective for efferent function, but intensity is key. Proprioceptive training, TENS, and cryotherapy improve somatosensory function. Increasing the complexity of proprioceptive training (task type, visual info, cognitive load, perturbations) may help reduce visual-motor reliance.
Referanse
LÆR Å OPTIMERE REHAB OG RTS-BESLUTNINGER ETTER ACL REKONSTRUKSJON
Registrer deg for dette GRATIS webinaret og topp ledende ekspert på ACL-rehab Bart Dingenen vil vise deg nøyaktig hvordan du kan gjøre det bedre i ACL-rehab og gå tilbake til sportsbeslutninger

