Beyond The Foot: Exploring Associations Between Neuropathic Symptoms or Catastrophizing and Chronic Plantar Fasciopathy

Introduksjon
Chronic plantar heel pain or plantar fasciopathy can be a stubborn condition to treat. It has been assumed that the condition is self-limiting in nature, which has often led to the recommendation of wait-and-see approaches. Recently, a prospective study highlighted ongoing symptoms in about half of their studied population in a 10 (!) year follow-up. It appears that not everyone will see the symptoms disappear based on a self-limiting natural course, and that recovery trajectories differ between individuals. Known influencing factors include some unmodifiable demographic factors, such as BMI or gender. Little is known about modifiable factors that treatment can target. Therefore, this study examined clinical factors in a biopsychosocial framework and assessed how their changes are associated with changes in chronic plantar heel pain, function, and quality of life over 12 months. This way, the current study looked beyond the foot by exploring associations between modifiable biopsychosocial factors such as the presence of neuropathic symptoms, ankle plantar flexor strength, or pain catastrophizing, and chronic plantar fasciopathy.
Metoder
The researchers used a prospective cohort study with longitudinal follow-up over 12 months in a community setting in southern Tasmania. Participants were people with a clinical diagnosis of chronic plantar heel pain.
Participants aged 18 years and older with pain under the heel aggravated by weight-bearing function that has lasted for at least 3 months were included. The most symptomatic heel was assessed in case of bilateral symptoms. Participants were excluded if they reported a history of prior foot/ankle fracture or orthopedic foot surgery, current ankle pain, recent foot trauma, or other conditions limiting mobility or activity within the preceding three months. Exclusion also applied to those who had received a corticosteroid or other injection, shock wave treatment, or steroid iontophoresis within the previous six months.
Outcomes and exposures were assessed at baseline and 12 months. The key clinical factors measured were:
- Pain Catastrophizing Beliefs were assessed using the Pain Catastrophizing Scale (PCS). A score greater than 20 was considered clinically important pain catastrophizing.
- Neuropathic Symptoms were measured using the painDETECT questionnaire (score range 1 to 38). A score of 19 or more was used to indicate a “probably neuropathic” component to pain.
- Physical measures obtained were:
- Body Mass Index (BMI, kg/m²) and Waist Circumference (centimeters).
- Maximum Isometric Ankle Plantarflexor Strength (kilograms), measured in sitting with the lower limb strapped by a nonelastic belt around the knee to a digital scale.
- Ankle and first metatarsophalangeal joint (MTPJ) dorsiflexion mobility (degrees), measured with a gravity inclinometer on the mid-anterior shin and goniometric measurements with the foot plantigrade in the supine position, respectively.
- Psychological/Symptom Descriptors captured were:
- Depression: Assessed with the 9-item Patient Health Questionnaire (PHQ-9).
- Multisite Pain: Recorded by checklist as the sum of body region pain sites other than the heel, ranging from 0 to 7.
- Morning Stiffness symptoms and Comorbidities (diabetes, rheumatological disease).
- Physical Activity: Measured with a uniaxial accelerometer worn at the waist for 7 consecutive days, reporting steps per day, and minutes in moderate to vigorous, light, and sedentary activities.
Main outcomes were Foot Pain and Function, which were assessed using the pain and function domains of the Foot Health Status Questionnaire (FHSQ). Scores range from 0 to 100, where higher scores represent less pain and better function. An improvement of at least 13 points was considered to meet or exceed the minimal important difference for the pain domain. Quality of Life was measured with the 6-dimensional Assessment of Quality of Life Scale (AQoL-6D). Scores range from 0 to 100, where higher is better.
Resultater
The study collected data from 220 participants at baseline, of which 210 returned the surveys, and 202 attended clinical reassessment at a minimum of 1 year later. The median time to follow-up was 406 days from the initial assessment (interquartile range 373 to 430 days). The evolution in the mean FHSQ pain scores noted an increase from 48.8/100 to 75.9/100, indicating a decrease in pain. Foot function improved by 31% from 65.7 to 86.13, and quality of life improved from 76.4 to 81.6, which is 7%.
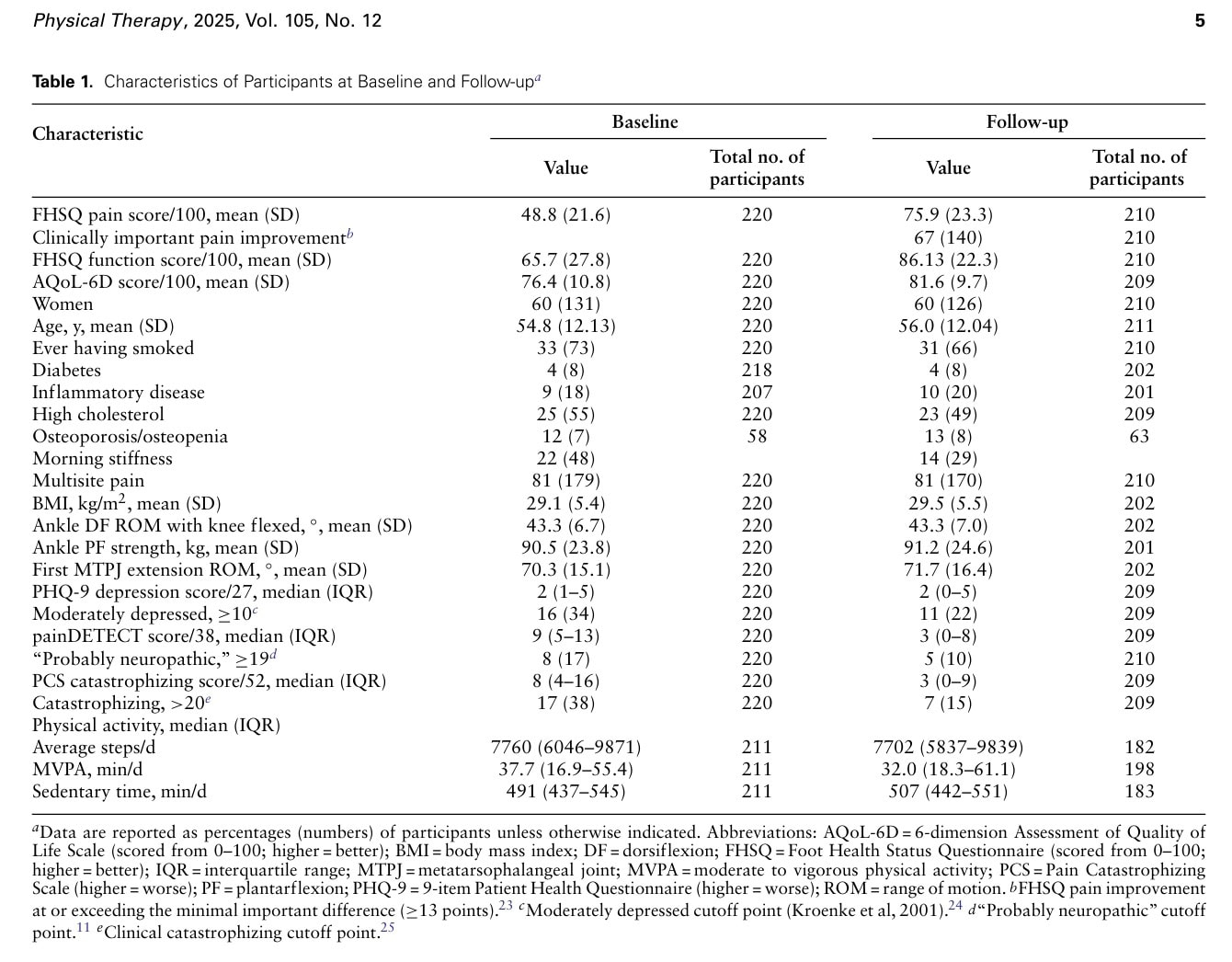
At the follow-up, 21% of participants reported no longer experiencing plantar heel pain, 67% indicated pain that improved by at least the minimal clinically important difference of 13 points. The authors noted that at baseline 21% of participants reported receiving treatment, compared to 7% at follow-up.
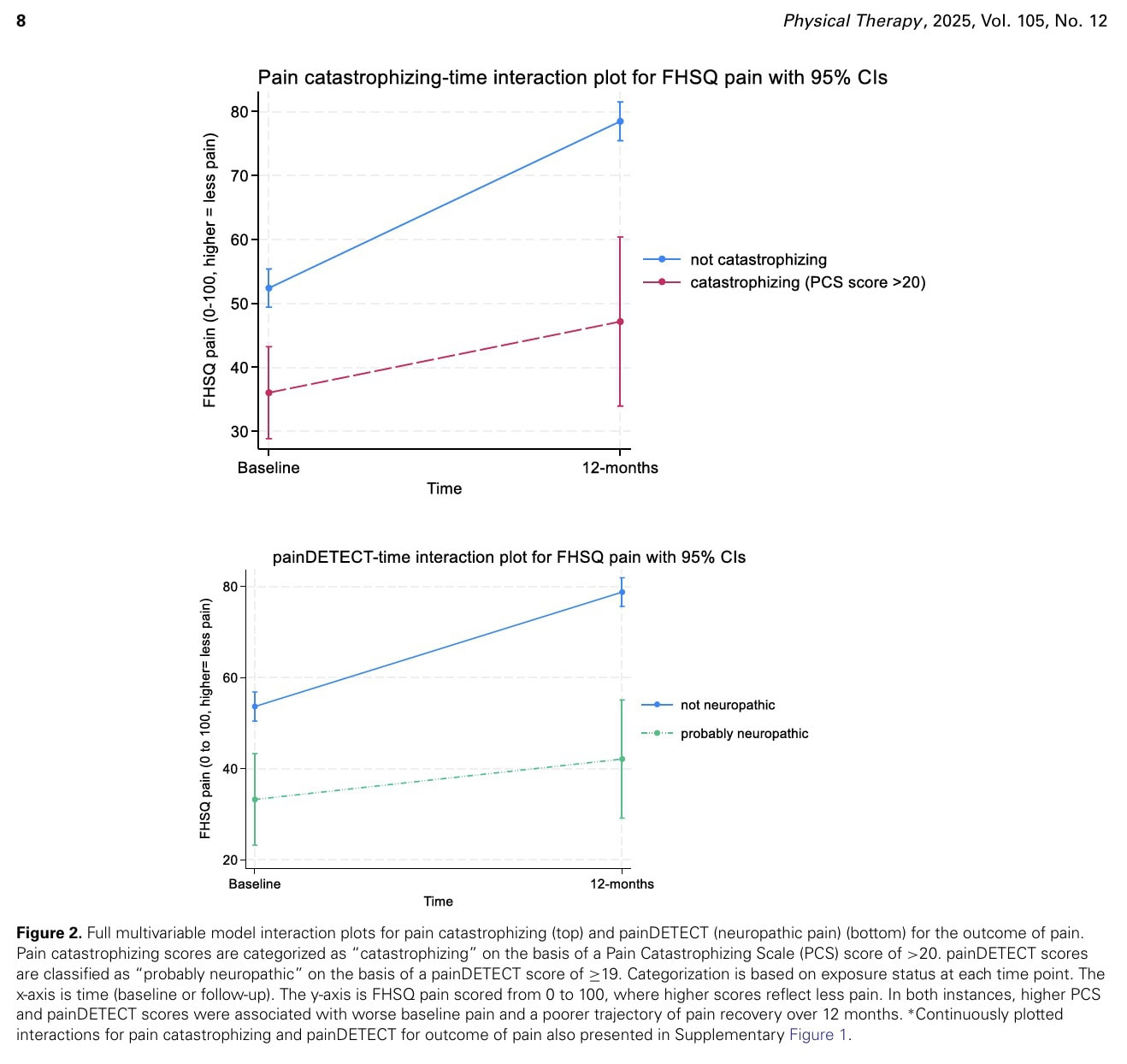
In the fully adjusted multivariable models, an increase in both the painDETECT and pain catastrophizing scores was associated with less improvement in pain over 12 months (interaction β = −.79 [95% CI = −0.10 to −1.48] and interaction β = −.39 [95% CI = −0.01 to −0.77], respectively).
Higher scores in these outcomes were associated with worse baseline pain scores that improved less over 12 months when the outcomes indicated the presence of catastrophic beliefs (PCS > 20) (interaction β = −15 [95% CI = −28.5 to −1.4]) or as “probably neuropathic” (painDETECT ≥ 19) (interaction β = −15.8 [95% CI = −29.9 to −1.7]).
Catastrophizers had less pain resolution compared to non-catastrophizers. People who had a “probably neuropathic” pain presentation also had less pain improvement over 12 months compared to people not having neuropathic symptoms.
No other variables (BMI, waist girth, ankle plantarflexor strength, multisite pain, physical activity) showed a significant association with the trajectory of pain. The authors also examined the associations between their proposed exposures and foot function or quality of life, but these associations were nonexistent or only weak (steps per day with function and sedentary time with quality of life).
Spørsmål og tanker
Since this was a cohort study, no causal links can be established. Nevertheless, the study deserves praise for looking beyond the foot alone. By integrating modifiable factors into a biopsychosocial framework, the observed associations form a practical starting point for future research. Since we can influence these factors, for example, by applying pain education to address maladaptive beliefs such as catastrophizing, randomized controlled trials can be effectively designed to confirm or refute the observations. Previous studies have not focused as much on modifiable factors, making it less practical for clinicians to be certain of their influence.
The included participants were affected by chronic plantar heel pain for at least 3 months, which may limit the generalizability of the observations to more acute cases. Yet, the finding that the presence of neuropathic symptoms at baseline or catastrophizing and chronic plantar fasciopathy may be intertwined opens new perspectives for the initial management of these individuals. As this study has observed that people who tended to catastrophize didn’t see as much improvement in their pain as those who didn’t, plus patients whose pain seemed “probably neuropathic” didn’t get as much relief over a year compared to those without those neuropathic signs, this signals that the initial correct classification of these individuals should be prioritized. Probably, these patients are the ones who should be seen in a more multidisciplinary care setting.
No associations were found between the exposures and foot function and foot-related quality of life. This may be due to the fact that function and quality-of-life measures started at a relatively good baseline level and changed less than pain, suggesting potential ceiling effects and reduced variability, which could make it difficult to detect change in these outcomes.
Snakk nerdete til meg
The data were analyzed using Linear Mixed-Effects Models. This statistical approach was used to estimate how changes in each clinical exposure over 12 months affected changes in the outcomes (pain, function, quality of life) over the same period. These models include a random intercept for individuals to account for the fact that repeated measurements on the same person are correlated. The researchers included an exposure x time interaction term in their models. Basically, this term was to test their primary goal: seeing if the exposure’s effect on the outcome changed between the start and the follow-up. This lets them check out the time-dependent shift in the outcome when the exposure changed. Given the observational nature of this cohort study, the results can only demonstrate an association between factors like pain catastrophizing and poorer outcomes; they cannot establish a causal relationship.
Individuals categorized as catastrophizers exhibited less favorable pain resolution compared to their non-catastrophizing counterparts. Furthermore, participants presenting with “probably neuropathic” pain symptoms experienced less significant pain improvement over the 12 months in comparison to those without neuropathic symptoms. These observed pain trajectories were highlighted as being large enough to be clinically relevant since they exceeded the MCIDs, yet the confidence intervals were wide, indicating that this may be true for some, but not for all. The document mentions that effects were considered relative to the MCID for each outcome (where known), but it does not explicitly state the numerical MCID values for the other main outcomes, which were the FHSQ function and the 6-dimensional Assessment of Quality of Life Scale (AQoL-6D).
A limitation includes the use of the painDETECT questionnaire, which was originally validated in a low back pain population and seeks to differentiate nociceptive from neuropathic pain. Firstly, this tool was developed before the recognition of nociplastic pain. Secondly, it can be questioned whether the proposed cutoff score of 19 to classify pain as “probably neuropathic” is the optimal threshold for this population. The authors acknowledge that it may be possible that this also captures features of nociplastic pain.
Another limitation lies in the tracking of the physical activity data, which was measured by wearing a uniaxial accelerometer, which may entail an increased risk of unmeasured activities taking place in other directions (tennis, gardening, dancing, etc). While physical activity was measured with accelerometry, the authors note that higher quantities of both average steps per day and moderate-to-vigorous physical activity were associated with better function/quality of life at baseline, but the statistical interaction suggested a poorer recovery of function/quality of life. The authors suggest this may be “regression to the mean,” but a deeper look into the behavioral consequences of pain/catastrophizing on activity levels might be warranted
Ta med hjem meldinger
This study followed people with chronic plantar heel pain for a year and found that their pain recovery was significantly worse if they reported worsening negative thoughts about their pain (catastrophizing) or worsening nerve-related symptoms (neuropathic pain). This suggests that a patient’s mindset and neurogenic profile are much more important for long-term pain resolution than traditional factors like their BMI, ankle strength, or general multisite pain. The biggest threat to the validity of the conclusions is that the study is observational. It only shows that these factors are associated with poor outcomes; it does not prove they are the cause.
Referanse
Hvordan ernæring kan være en avgjørende faktor for sentral sensibilisering - Videoforelesning
Se denne GRATIS videoforelesningen om Nutrition & Central Sensibilization av Europas #1 kroniske smerteforsker Jo Nijs. Hvilken matpasienter bør unngå vil nok overraske deg!

