Arthroscopic Partial Meniscectomy or Exercise for Degenerative Meniscus Tears - Results From a 10-Year Follow-Up

Uvod
Degenerative meniscal tears are common among middle-aged and older adults. While arthroscopic partial meniscectomy (APM) has long been the standard treatment, recent studies suggest that exercise therapy may offer similar or even superior results without the risks associated with surgery. Despite this growing body of evidence favoring exercise, follow-up data beyond five years remains sparse. Additionally, the long-term impact of both treatment options on knee osteoarthritis (OA) development in middle-aged individuals with degenerative meniscal tears remains uncertain. This randomized controlled trial bridges these research gaps by comparing the long-term effects of APM and exercise on knee OA progression and overall knee function at a 10-year follow-up.
Metode
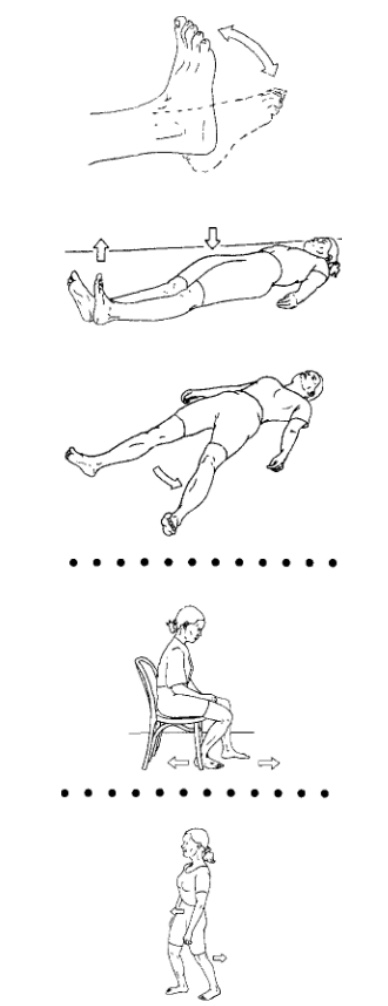
Participants were recruited from two hospitals in Norway and were randomised to either APM or exercise in a 1:1 ratio. Eligible patients were aged 35-60 years, experienced nontraumatic unilateral knee pain for over two months and had a confirmed medial degenerative meniscal tear. Additionally, participants had no or minimal radiographic signs of knee OA, corresponding to a maximum of Kellgren and Lawrence (K&L) grade 2. The K&L scale classifies knee OA severity from 0 (normal) to 4 (severe). Patients randomised to the APM group underwent resection of unstable meniscal tissue and received postoperative instructions, including light movement exercises aimed at regaining joint range of motion and reducing swelling. The exercises are illustrated below.
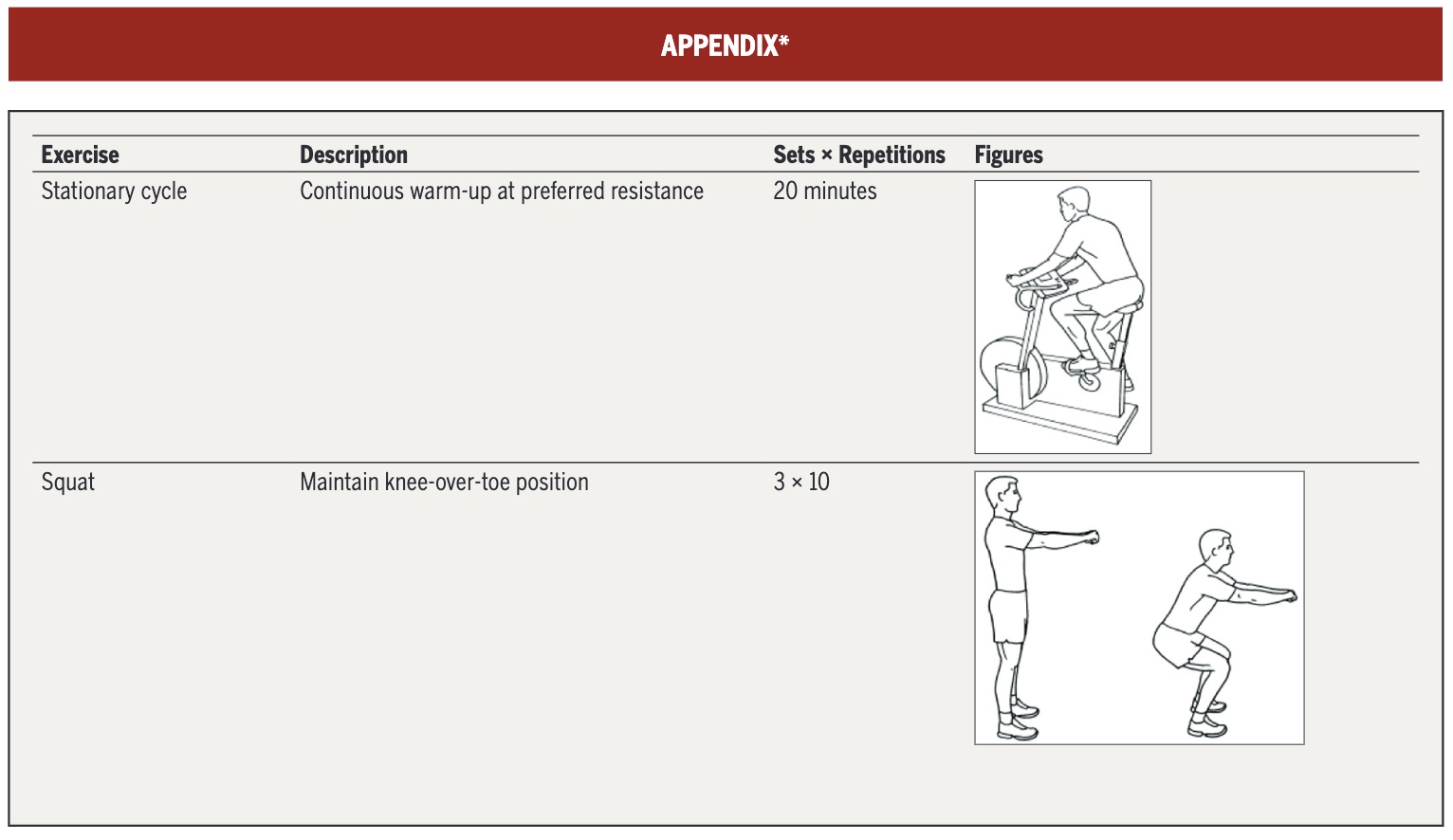
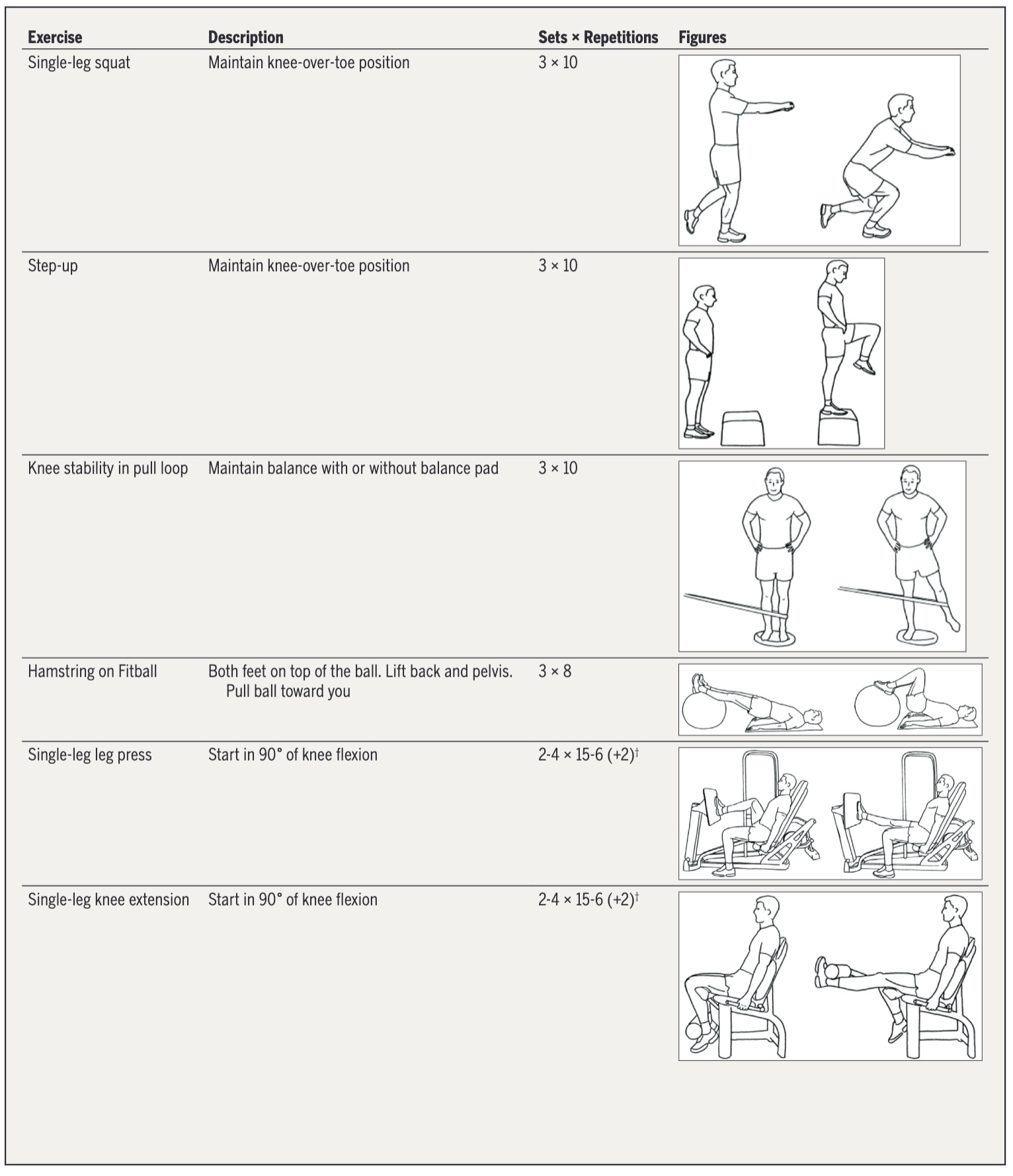
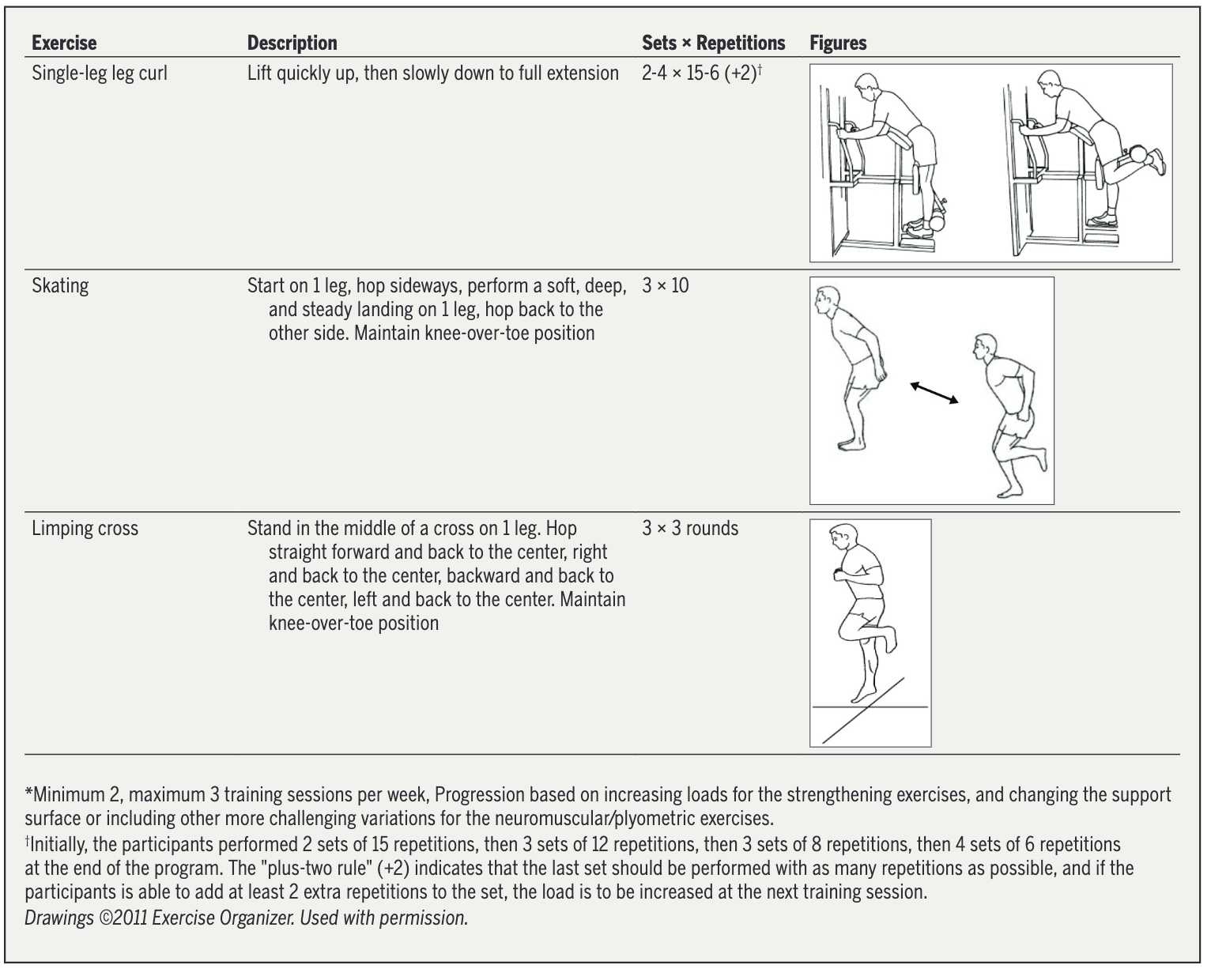
Patients randomised to exercise performed treatment sessions 2 to 3 times per week for 12 weeks in a physiotherapy clinic, with 1 weekly session supervised by a physical therapist. The treatment program consisted of progressive strength exercises and neuromuscular exercises aimed at improving balance and functional stability of the lower extremity. The exercises, their training variables and ways of progression are displayed below.
The primary outcome was radiographic knee OA progression assessed by the change from baseline in the Osteoarthritis Research Society International (OARSI) atlas sum score at 10 years. It assesses joint space narrowing and osteophytes in the tibiofemoral joint. The OARSI sum score ranges from 0 (normal) to 18 (severe OA). A secondary outcome was radiographic knee OA incidence, defined as the emergence of K&L grade ≥2 at 10 years in knees graded 0 or 1 at baseline. Participants with incident radiographic knee OA experiencing knee pain at least weekly were classified as having symptomatic knee OA.
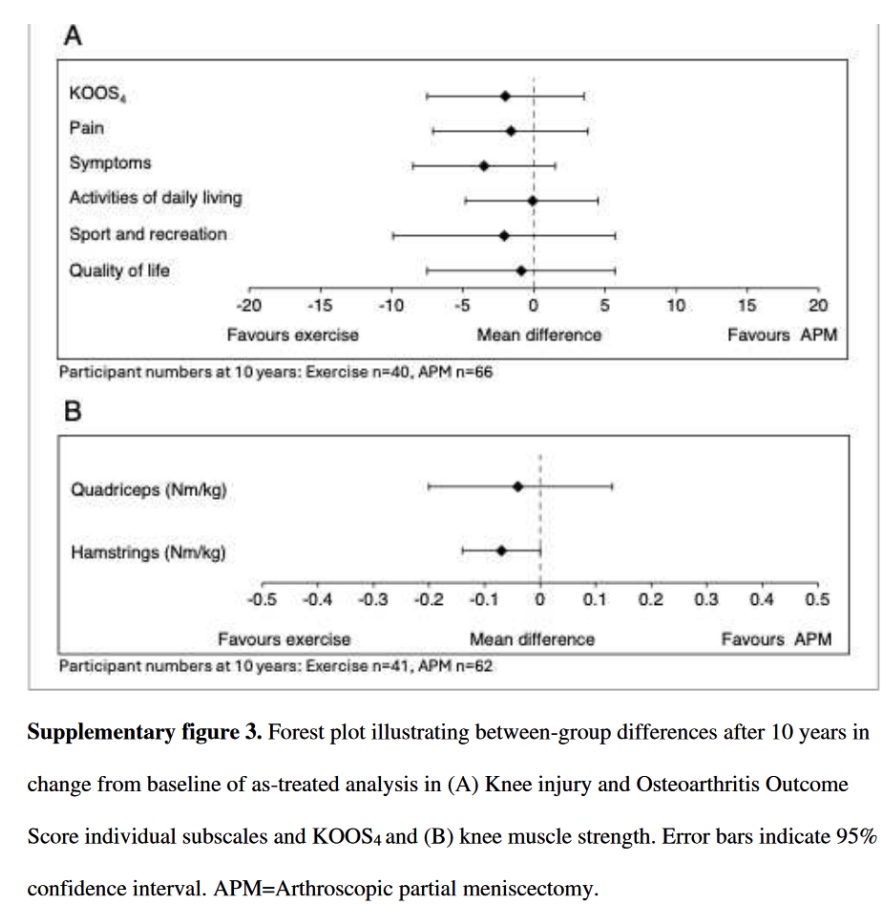
Patient-reported outcomes were assessed by changes from baseline in the five subscales of the Knee Injury and Osteoarthritis Outcome Score (KOOS): pain, symptoms, ADL, sport/recreational function, and quality of life. KOOS4, a composite score from all subscales excluding ADL, was also compared. KOOS values range from 0 (extreme knee problems) to 100 (no knee problems). Finally, changes from baseline in quadriceps and hamstrings muscle strength were assessed and compared using an isokinetic dynamometer. For continuous outcomes (OARSI score, KOOS score, and muscle strength), participants’ data were analysed based on their original treatment allocation, using the intention-to-treat (ITT) design. Binary outcomes (knee OA incidence) were analysed using the full analysis set (FAS), excluding patients with missing data. Additionally, due to treatment crossover, an as-treated analysis was conducted, in which the APM group included patients who crossed over from the exercise group. The two radiographic assessors were blinded to the group allocation of the patients.
Rezultati
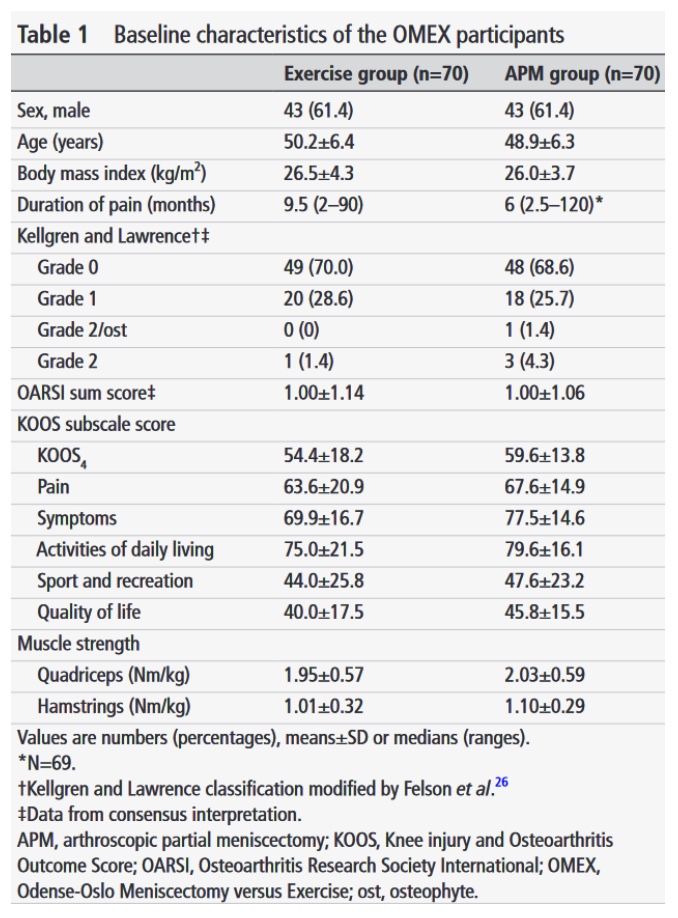
140 patients were included in the trial. The two groups show comparable characteristics at baseline.
Of the participants allocated to exercise, 14 (20%) crossed over to receive APM before the 2-year follow-up. No participants in the APM group crossed over to exercise.
Loss to follow-up
At the 10-year follow-up, of the 70 participants originally allocated to each group, the remaining number of participants provided data:

Missing values caused by loss to follow-up were statistically estimated for the analyses of continuous outcomes.
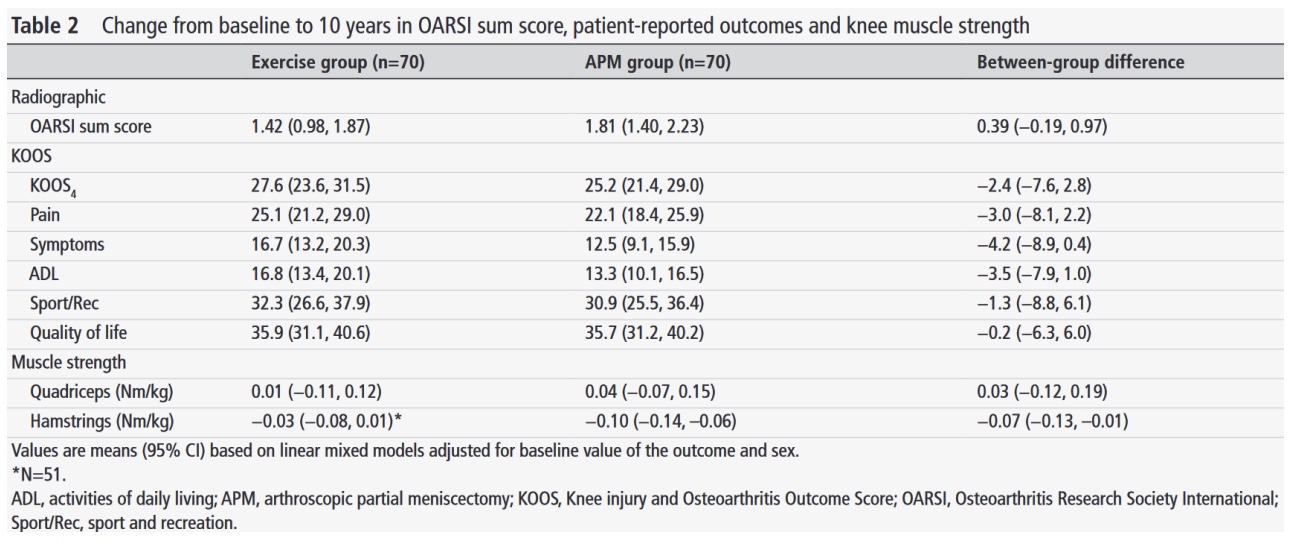
OARSI Score
At 10 years, the mean OARSI sum score increase showed mild OA progression, with 1.81 (95% CI 1.40 to 2.23) for APM and 1.42 (95% CI 0.98 to 1.87) for exercise. Given the small absolute magnitude accumulated over a decade, these changes are unlikely to be clinically meaningful. However, no validated MCID has been established for the change in OARSI sum score. The between-group difference in OARSI change was 0.39 (95% CI −0.19 to 0.97) in the ITT analysis and 0.57 (95% CI −0.05 to 1.20) in the as-treated analysis, slightly favoring exercise, but neither difference was statistically significant, indicating similar radiographic OA progression for both treatments.
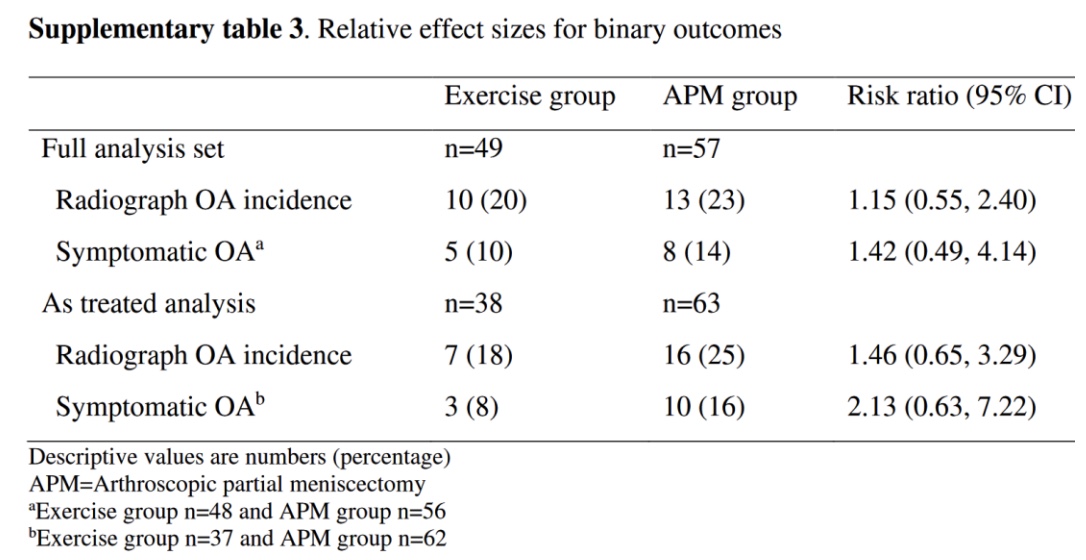
OA incidence
The incidence of radiographic and symptomatic knee OA was similar in both groups. Although the risk ratios and between-group risk differences indicated a slightly lower risk of OA incidence in the exercise group, the differences were almost never clinically relevant and did not reach statistical significance.
Patient-reported outcomes
Both groups reported substantial improvements over the 10-year follow-up period. In the primary analysis, the between-group difference of every KOOS subscale marginally favored the progress achieved in the exercise group. But neither of these differences reached statistical significance or clinical relevance, indicating similar results irrespective of treatment option.
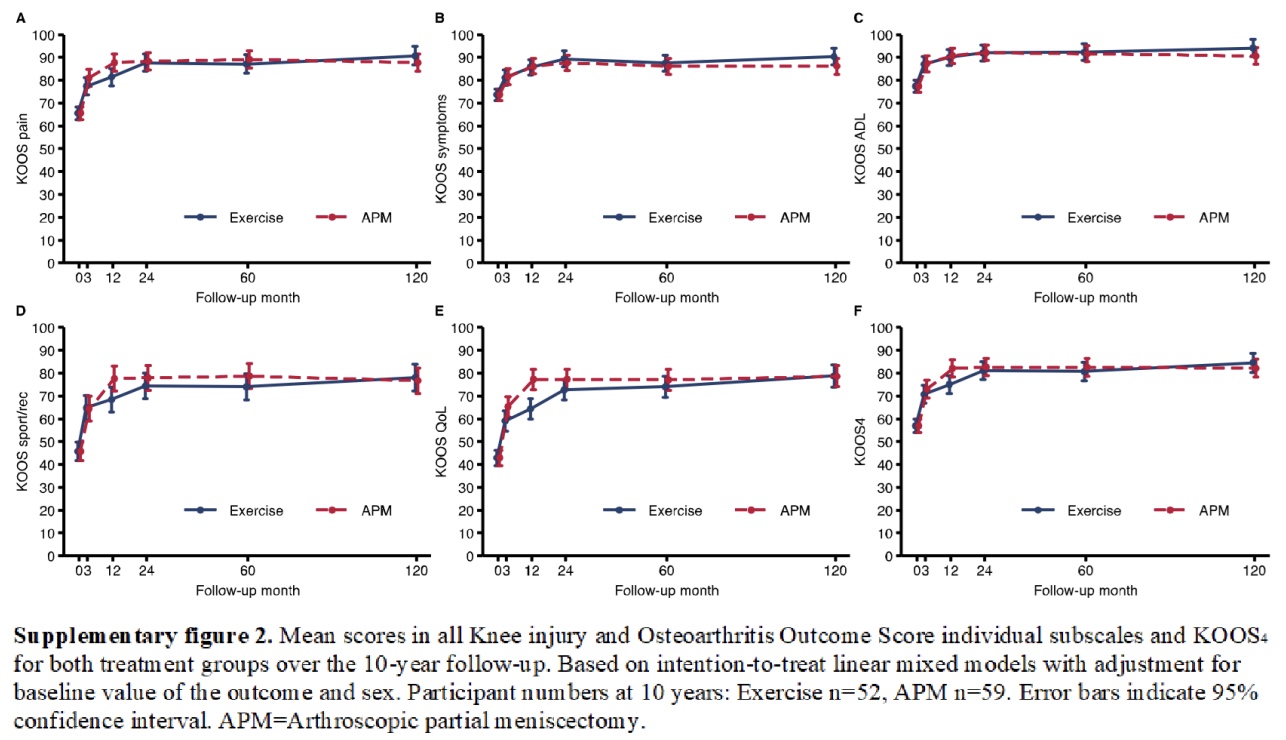
These results are consistent with the results of the as-treated analysis shown in the forest plot below.
Knee muscle strength
No meaningful changes in muscle strength were observed from baseline to 10 years. The only statistically significant between-group difference was the decline of −0.07 (95% CI −0.13 to −0.01) in hamstring muscle strength. While this indicates that the exercise group experienced less strength loss than the APM group, this between-group difference is trivial.
Pitanja i razmišljanja
This study is special for its extended follow-up duration, addressing the lack of long-term data in this area and offering clearer guidance for clinical decision-making. Along with earlier follow-up assessments of this trial, the development and progression of outcomes are displayed over the course of time. Nevertheless, the study has some limitations. The long follow-up is accompanied by a drop-out of 18-20 participants (25.7-28.6%) in the exercise group and 11-14 participants (15.7-20%) in the APM group, depending on the measured outcome. This increases the uncertainty of the results, despite using statistical methods to handle the missing data.
Participants were classified as having symptomatic knee OA when they had incident radiographic knee OA and experienced knee pain ‘at least weekly’. This criterion is somewhat broad. It’s possible that patients with radiographic knee OA experience regular, low-frequency knee pain due to causes other than the OA.
Both APM and exercise showed similar improvements in patient-reported outcomes and previous studies have shown that APM was no more effective than sham surgery for similar outcomes. Due to the absence of a third control group, it remains unclear how much of the observed improvement in both APM and exercise could be attributed to the placebo effect. Regarding external validity and generalizability, the study only recruited patients with minimal or no radiographic knee OA and medial meniscal lesions, so the findings may not necessarily apply to those with more severe OA or lateral meniscal lesions. Additionally, the outcomes of exercise may depend on the choice of exercises. The program in this study included progressive resistance training and challenging neuromuscular exercises for balance and functional stability, whereas a program with only machine-based strength exercises might lead to less favorable outcomes. Furthermore, during the 12 weeks of the intervention, the exercise group experienced greater strength gains compared to the APM group, but these gains declined after the intervention ended. It is plausible that extending the exercise intervention beyond 12 weeks could lead to improved outcomes.
The authors mention the unclear clinical relevance of radiographic changes (such as a 1 OARSI grade difference) in individuals with degenerative meniscal tears and early OA. Imaging findings don’t always match up to the patient’s symptoms. Even in this study, a noticeable amount of the patients classified as having radiographic OA did not report having regular knee pain. At 10 years, only 50% (5/10) of radiographic OA patients reported having regular knee pain in the exercise group and 62% (8/13) in the APM group (see supplementary table 3 in results above). Therefore, while the primary outcome of this study relates to the radiographic OARSI sum score, what matters most are the clinical outcomes of the patients, e.g., quality of life, knee function, and pain.
Pričaj štreberski sa mnom
For the continuous outcomes, missing patient data at 10 years were statistically estimated, allowing for a full analysis with 70 participants in each group in the ITT analysis. On the other hand, for binary outcomes (knee OA incidence), patients with missing data were excluded from the FAS analysis, as inaccurate imputation of binary variables can more significantly distort the results. For example, if the presence or absence of knee OA at 10 years is misclassified in a participant with missing data, it can have a greater negative impact on the outcome than a small error in estimating a continuous variable like the KOOS score.
No a priori sample size calculation was performed for the 10-year follow-up. As patients with missing data were excluded from analysis of binary outcomes, the authors note that the sample size was too small to analyse the development of radiographic and symptomatic knee OA with sufficient statistical power, leading to uncertain results in the between-group differences. Nevertheless, for the OARSI sum score, KOOS scales, and muscle strength, the confidence intervals were narrow enough to rule out clinically relevant differences between APM and exercise.
Fourteen patients (20%) crossed over from exercise to APM. In the primary analysis, however, patient data were analysed based on their original group allocation, which may have distorted the true effect of APM and exercise. Therefore, an as-treated analysis was conducted, which largely confirmed the non-significant results of the primary analysis, though differences in the OARSI score and knee OA incidence favored exercise slightly more than in the primary analysis.
As shown in the results, nearly all between-group differences for the analysed outcomes favored exercise, albeit mostly not statistically significant, making it seem like exercise marginally outperformed APM in total. However, it’s still important to note that almost none of these differences were clinically relevant.
Poruke za ponijeti kući
10 years following APM or exercise for degenerative meniscal tears, there were no essential between-group differences in the development and progression of radiographic knee OA or improvements in clinical outcomes related to knee function. This study provides further evidence that exercise is at least as effective as APM in managing degenerative meniscal tears, offering a safer, non-invasive treatment alternative, reducing the risks associated with surgery.
Referenca
ULOGA VMO-a & QUAD-ova U PFP-u
Pogledajte ovo BESPLATNO VIDEO PREDAVANJE U 2 DIJELA stručnjakinje za bolove u koljenima Claire Robertson koja secira literaturu o toj temi i kako ona utječe na kliničku praksu .

